Category: Dog Health
Great Pet Care - Pet health information — simplified.
5 Canine Heart Problems to Know About
- 2025-03-11T13:46:19
- Catherine Barnette, DVM
Heart disease is a relatively common condition in dogs, especially in older dogs. In fact, it is estimated that approximately 10 percent of dogs seen by primary care veterinarians have some form of heart disease [1]. There are multiple types of heart disease in dogs, each with their own unique causes and treatment. Read on to learn more about common canine heart problems.
What Causes Heart Problems in Dogs?
Heart disease in dogs, also known as cardiac disease, can have a number of potential causes.
Most canine heart disease is age-related. As dogs age, the valves within their heart may weaken and deteriorate. This prevents the heart valves from closing normally. Instead of blood flowing smoothly through the four chambers of the heart, a leaky heart valve can allow backflow within the heart, with some blood not moving forward along its normal path. Age-related valve degeneration is the most common cause of heart disease in dogs.
Some cases of heart disease are congenital, meaning the dog is born with a heart defect. This defect may be diagnosed at a puppy’s first veterinary exam, or it may be inapparent until later in life. Examples of congenital heart disease include patent ductus arteriosus (in which an embryonic heart vessel fails to close at birth), septal defects (presence of an abnormal opening that connects the left and right sides of the heart), and pulmonic stenosis (abnormally narrow pulmonic valve within the heart).
Less common causes of heart disease in dogs include viral infections, bacterial infections, tumors, nutritional deficiencies, hormonal disorders, and obesity.
Some breeds are more likely to develop heart disease than others. For example, Cavalier King Charles Spaniels almost always develop heart disease at some point during their lives. Other breeds that are predisposed to heart disease include Miniature Schnauzers, Toy Poodles, Chihuahuas, Shih Tzus, Boxers, and Doberman Pinschers.
Signs of Dog Heart Problems

Heart disease is often asymptomatic or nearly asymptomatic in their early stages. Your veterinarian may notice signs of heart disease on a physical exam, but these signs may not be obvious at home. Signs that your veterinarian may notice on their exam include:
- Heart murmur
- Abnormal heart rhythm (arrhythmia)
- Abnormal pulses
As heart disease progresses, you may start to see signs at home. Signs of heart problems in dogs may include:
- Coughing
- Increased respiratory rate
- Exercise intolerance
- Fainting
Congestive heart failure (CHF) is a late stage of heart disease. Dogs develop CHF when their body can no longer compensate for their heart disease. Signs of CHF include:
- Shortness of breath
- Difficulty breathing
- Cough (especially a productive cough)
- Blue tinge to gums
- Swollen belly due to fluid accumulation
- Weak pulse
- Lethargy
If your dog is showing signs of heart disease, schedule an appointment with your veterinarian. Your veterinarian will begin by performing a thorough physical exam, listening to your dog’s heart and lungs, palpating their pulses, and checking your dog carefully for other health issues.
If your dog’s exam suggests a possibility of heart disease, your veterinarian will likely recommend additional testing. These tests may include an electrocardiogram (ECG), chest X-rays, and/or an echocardiogram (ultrasound of the heart).
5 Canine Heart Problems to Know About

There are numerous forms of heart disease in dogs. Each type of heart disease is different in its underlying cause, its impact, and its treatment.
Here are five common heart diseases that affect dogs:
Mitral valve disease (MVD)
Mitral valve disease is the most common heart disease in dogs. The mitral valve separates the left atrium from the left ventricle of the heart. As dogs age, this valve can begin to deteriorate and become leaky over time. This means that blood isn’t pushed out of the heart normally when the heart beats; instead, some of the blood may leak from the ventricle back into the atrium. This forces the heart to work harder, leading to signs of heart disease.
While leaky mitral valves are typically repaired or replaced in people, this is not feasible in dogs. Therefore, MVD is managed, not cured. Your veterinarian will prescribe heart medications to support your dog’s heart function, as well as medications to prevent or treat the congestive heart failure that can occur secondary to mitral valve disease.
Congestive Heart Failure (CHF)
Congestive heart failure is a late-stage effect of any form of canine heart disease. When the heart cannot effectively move blood forward, fluid may begin to pool within the lungs and other parts of the body. This can lead to a variety of signs, such as difficulty breathing, a bloated or round appearance to the abdomen, and edema (fluid) in the legs.
The treatment of CHF involves removing this extra fluid from the body and the lungs. Veterinarians typically prescribe a diuretic, such as furosemide. More medications may also be prescribed to treat the underlying cause of CHF and otherwise support heart function.
Heartworm Disease

Heartworm disease is caused by a parasite, Dirofilaria immitis. This parasite is spread by mosquitoes. In fact, a single mosquito bite is all that it takes to spread heartworms to an unprotected dog.
Although heartworm larvae start off as small, microscopic parasites, they mature into large worms that look like spaghetti. These worms lodge within a dog’s heart and lungs, blocking normal circulation. Fortunately, heartworm infection can be prevented with the use of year-round heartworm preventative.
Dilated cardiomyopathy (DCM)
Dilated cardiomyopathy is a condition in which the heart muscle becomes weakened. This leads to enlargement of the heart, as the walls of the heart grow thinner and lose their normal shape. This condition is most common in large breed dogs, such as Great Danes, Boxers, and Doberman Pinschers. Diet can also play a role in the development of DCM, causing it to occur in breeds that are not commonly affected by this condition.
There is no cure for DCM. Instead, veterinarians prescribe medications to support heart function, reduce fluid buildup within the body, and reduce the risk of arrhythmias.
Pulmonic stenosis (PS)
Pulmonic stenosis is an inherited heart defect in which the valve between the right ventricle and the pulmonary artery (the vessel that carries blood to the lungs) is narrowed. This means that the heart must work harder to pump blood through this narrowed valve.
Pulmonic stenosis is treated with balloon valvuloplasty. This surgical treatment opens the valve up to a more normal width, restoring unobstructed blood flow.
Canine Heart Health: How to Stay Ahead of Problems

The most preventable cause of heart disease is heartworms. These parasites are spread by mosquitoes, and a single bite can be enough to cause life-threatening disease. Talk to your veterinarian and ensure that your dog is on year-round heartworm prevention to prevent heartworm disease.
Some cases of heart disease are nutritional in nature. Feeding an imbalanced diet can increase your dog’s risk of heart disease. Therefore, it’s important to talk to your veterinarian and ensure that you are feeding a nutritionally complete and balanced diet that’s appropriate for your dog’s life stage. If your dog is at increased risk of heart disease, or is already showing signs of heart disease, your veterinarian may recommend a cardiac diet or nutritional supplement.
If you are considering a purebred dog, do your homework. Some breeds are more likely to develop heart disease than others; avoiding these breeds can reduce your risk of adopting a dog with heart problems. If you’re purchasing a dog from a breeder, consult the Orthopedic Foundation for Animals’ recommended list of breed-specific screenings to determine whether cardiac screenings are recommended for that breed. Do not buy a puppy unless the breeder can verify that the puppy’s parents received and passed the recommended screening tests for their breed.
Unfortunately, most cases of heart disease cannot be avoided or prevented. Instead, it’s important to pay close attention to your dog and ensure that they receive regular veterinary care. Early diagnosis of heart disease allows early treatment, potentially improving your dog’s prognosis.
Reference
- Keene, Bruce W et al. “ACVIM consensus guidelines for the diagnosis and treatment of myxomatous mitral valve disease in dogs.” Journal of veterinary internal medicine vol. 33,3 (2019): 1127-1140. doi:10.1111/jvim.15488
Understanding Dog Blood Test Results
- 2025-02-09T19:50:59
- Sarah J. Wooten, DVM
Blood tests are routinely used by veterinarians to monitor a dog’s health or help diagnose medical conditions. But often the results of a dog blood test, or the reasons why a test is being run in the first place, can be confusing for pet parents to understand, so let’s try and clear things up for you.
In this article, you will learn why dogs need blood tests, the most common types of blood tests in dogs, how to understand blood test results, and how much testing generally costs.
Why Do Dogs Need Blood Tests?
Veterinarians can gain a wealth of information about the health of a dog by running different blood tests.
At your dog’s last annual examination, your veterinarian may have recommended running routine bloodwork to check the health of blood cells and internal organ function. The reason for this is even though a dog may look and act healthy on the outside, they may have hidden problems “under the hood.” Testing allows veterinarians to detect problems early when they are small and intervene to stop or slow the progression of disease. Having your dog’s blood tested annually can also help your veterinarian track health trends over time and know what is “healthy” for your dog if they ever get sick.
Another reason your veterinarian will recommend or require routine bloodwork is if your dog is receiving certain medications over a long period of time or about to start a new medication. For example, if your dog is regularly receiving a non-steroidal anti-inflammatory drug (NSAID) like carprofen, your vet may require bloodwork before refilling the medication. Bloodwork for medication varies but usually checks liver and kidney function and sometimes levels of medication in the blood. If you want to purchase heartworm prevention for your dog, your vet will run a heartworm test before they prescribe the medication.
Lastly, if your dog is going to be anesthetized for any reason, a veterinarian will often run routine blood tests to ensure that the dog is healthy enough for anesthesia.
In addition to routine bloodwork, a veterinarian will run blood tests if your dog is sick. Routine bloodwork can provide information about many diseases and conditions, including:
- Anemia
- Blood parasites
- Liver disease
- Kidney disease
- Protein losing diseases
- Inflammation
- Infection
- Auto-immune disease
- Dehydration
- Cancer
Types of Dog Blood Tests

Routine bloodwork typically consists of a few tests that can usually be run in-hospital for same-day results:
- Blood chemistry checks internal organ function, body electrolyte and fluid balance, blood proteins, blood sugar, minerals, and some enzymes
- Complete blood count, otherwise known as CBC blood test for dogs, checks red blood cells, white blood cells, and platelets
- Heartworm antigen test checks for the presence of heartworm disease
- 4DX blood test for dogs checks for four infectious diseases (heartworm disease, Lyme disease, ehrlichiosis, and anaplasmosis) carried by external parasites.
Additional blood tests that are not included in routine bloodwork can be run to further classify and diagnose a dog’s problem. There are many specialized blood tests for dogs available. Some tests can be run in-hospital for same-day results. Other tests must be run in a reference laboratory. Results for tests that are run at a reference laboratory take longer because the blood sample must be sent to the laboratory. Some of the more common specialized blood tests used by veterinarians include:
- T4, Free T4 by dialysis, and T3 – used to diagnose thyroid problems
- ACTH and low-dose-dexamethasone testing – used to diagnose Cushing’s syndrome
- Serological testing – used to determine vaccination/protection status of a dog against specific infectious diseases
- B-type natriuretic peptide (BNP) – checks a hormone that is released by heart muscles when they are stressed, used to monitor heart disease
- Spec cPL Test/Spec fPL Test – checks a hormone that is released by the pancreas when it is inflamed, used to diagnose pancreatitis
- Nu.Q Cancer Test – tests for seven common cancers found in dogs
- SDMA test for early detection of kidney disease
- Allergy testing
- DNA testing
Understanding Blood Test Results for Dogs

Trying to interpret dog blood test results can feel like trying to understand ancient Greek if you don’t know what you are looking for. While any and all blood tests for your dog should be interpreted with the guidance of a veterinarian, it can be helpful to at least understand the basics of blood test results.
First, let’s talk about blood tests that result in a numerical value. For every blood test that results in a number, there is a reference range that has been previously established as “normal.” The reference range is the result of testing many healthy dogs and averaging the results. Reference ranges are provided by the laboratory and do not vary based on individual dogs.
For example, the normal reference range for blood glucose (sugar) in dogs is 80-120 milligrams/deciliter (mg/dl) of blood. If your dog’s blood sugar falls within this range, they are considered to have normal blood sugar. Blood values that fall within their reference range and are “normal” will usually show up as green on printed lab work. If a dog’s blood sugar is outside this range and is either too high or too low, then the result will be flagged with a red color, alerting the veterinarian that something isn’t right.
Interpreting blood test results isn’t as straightforward as it seems, however. A completely normal dog may have high blood sugar levels because they just ate. A dog may have low thyroid hormone levels because they are sick with something else, not because they are hypothyroid. Dehydration causes concentration of red blood cells in the blood, and blood tests on a dehydrated, anemic dog may come back with “normal” levels of red blood cells, even though the dog is clearly very sick. This is why it is very important for veterinarians to interpret blood test results in light of the dog’s overall condition and take into account anything that can affect test results.
Specialized testing, especially tests that are run in reference laboratories, will not only give a numerical result but also will provide additional context on how to interpret the results. Furthermore, if a veterinarian does not understand the results, they can call the laboratory to get more information.
In addition to tests that result in numerical values, there are blood tests that give spot results. The 4DX snap test is the most common spot test used for dogs in veterinary medicine. In this test, blood is mixed with a reagent and then pipetted onto a test kit. If the dog is infected, then blue spots will appear in the test window. These screening tests are interpreted subjectively like a pregnancy test, and are often followed up by additional testing.
Once blood tests have been run, a veterinarian will follow up with the pet parent to go over the results. Even if you don’t understand everything that is written on the printout, it is a good idea to keep a copy for your own records. You can also take notes on the paperwork while the veterinarian is talking. A veterinarian should show you all the results, both normal and abnormal, explain what the abnormal results mean, and provide guidance on what to do next.
Dog Blood Test Cost

The cost of testing varies based on what test is being run and where the test is being run. The cost of testing includes the cost of labor (paying the veterinary staff), supplies, and paying for the blood analysis machine or paying the reference laboratory for the test. Some testing is less expensive because the test is routine, easy, and the veterinary clinic uses that test for large volumes of patients. Other testing is more expensive based on how labor intensive the test is (for example a blood glucose curve requires day hospitalization, multiple blood draws, and then a veterinarian to analyze the results) or how much the reference lab is charging for the test.
In general, routine complete blood panels cost $100-$300. Specialized testing costs anywhere from $50-$400 or more, depending on the test. Veterinary care is an investment in your dog’s health, but it can be pricey. Pet parents have several options that they can use to offset the cost of veterinary care, such as pet insurance, line of credit, emergency credit card, or wellness plans offered through the veterinary clinic.
Dog Blood Test Benefits
Having your dog’s blood tested has many benefits that include early detection of disease, infectious disease control, ensuring safe anesthesia, and monitoring medication. Interpretation of blood tests is a nuanced skill that veterinarians develop by taking classes in clinical pathology and years of practice, which is why it is always important to work with a veterinarian you trust to interpret blood test results. By combining your veterinarian’s knowledge with modern lab technology, pet parents can help their dogs live longer, healthier lives.
Lethargic Dog: Causes and How to Help
- 2025-01-06T17:41:44
- Rhiannon Koehler, DVM, MPH
There’s a difference between a couch potato and a lethargic dog. While your couch potato dog may just be a tad lazy, a lethargic dog usually needs medical attention. Luckily, even a low-energy dog can signal to you that they’re not feeling like themselves.
Find out what canine lethargy is, potential causes, and the steps you should take to help your dog.
What Is Lethargy in Dogs?
Lethargy in dogs is defined as a decrease in energy and activity levels. If your dog is lethargic, you may notice they’re lounging around more than usual, uninterested in play, indifferent to walks, acting sluggish, and/or potentially not as interested in food as they typically would be.
While it’s normal for senior dogs to have a lower energy level than rambunctious puppies, that doesn’t mean that the senior dog is lethargic. Similarly, a low-energy Pug isn’t lethargic just because they don’t have the natural agility of a Border Collie!
Remember, lethargy involves a decrease in energy and activity compared with the individual dog’s usual baseline. “Lethargic” is not a synonym for “lazy,” “calm,” “reserved,” or “relaxed.”
Why Is My Dog Lethargic? Causes of Canine Lethargy

Your dog could be acting lethargic for a wide variety of reasons. Here, we’ll cover general reasons for a dog acting sluggish:
Infectious Disease
We experience lethargy when we’re sick, and our dogs are no different. Infections are usually bacterial, viral, fungal, or parasitic. Examples of infectious diseases that can cause lethargy in dogs include parvovirus, kennel cough, canine influenza, leptospirosis, heartworms, and hookworms.
Pain
Pain is an important cause of sudden lethargy in dogs. Pain can stem from arthritis, dental disease, injuries, intervertebral disc disease, and more. Unfortunately, your dog cannot easily tell you what hurts. Luckily, veterinarians are accustomed to figuring it out!
Chronic Health Conditions
Many canine health conditions include lethargy as a symptom. Examples include kidney disease, hypothyroidism, Cushing’s disease, diabetes, heart disease, and cancer. Chronic health conditions are generally more common in older dogs but can occasionally occur in young dogs.
Stress and Anxiety
While some dogs become more hyperactive when experiencing stress and anxiety, other dogs act withdrawn. Causes of stress and anxiety could include thunderstorms or fireworks, moving to a new home, a recent veterinary visit, a new pet or person in the home, lack of sufficient exercise or mental stimulation, and more.
Medications
Lethargy is a commonly listed side effect of many medications. Lethargy is often noted after a dog receives pain medications, anxiety medications, or sedatives. It’s also common for a dog to remain lethargic for around a day after undergoing anesthesia. While it’s possible for some antibiotics to make a dog tired, keep in mind that the underlying infection that the antibiotics are treating may also contribute to lethargy.
Vaccinations
Your dog may not feel quite like themself for a day or two after receiving a vaccination. Lethargy, achiness, and low grade fevers are normal side effects of recent vaccination.
Lethargic Dog Symptoms

Other symptoms that occur concurrently with lethargy could indicate that your dog is experiencing a medical issue. Examples of what to watch for include:
- Decreased or lost appetite
- Changes to the amount your dog is drinking
- Increased urination
- Vomiting and diarrhea
- Drooling
- Dropping food or difficulty chewing
- Acting weak or wobbly
- Hunched posture
- Pale or yellow mucous membranes (gums, whites of eyes, genitals)
- Sneezing, discharge from the eyes or nose, and/or coughing
- Difficulty breathing
- Limping
How to Help a Lethargic Dog: Next Steps

If you’re noticing your dog acting lethargic, the first thing you’ll want to do is observe them, taking note of any other symptoms that they’re exhibiting.
A dog acting lethargic with an obvious cause, such as recent vaccination or taking pain medications after surgery, may not be a cause for concern if they are otherwise still eating and acting okay.
If your dog has been acting lethargic for more than one day, you should contact your veterinarian. They may suggest bringing your pup in for an appointment to rule out pain, infections, and health conditions as causes.
Contact your veterinarian if your dog is experiencing other issues in addition to lethargy, such as vomiting, diarrhea, or limping. You should also contact your veterinarian if you have a lethargic puppy. Puppies are very susceptible to infectious disease and several other causes of lethargy. If your puppy is not eating much and sleeping a lot, talk to your vet.
If your dog is collapsing, has pale or yellow gums, is having difficulty breathing, or is showing any other serious symptoms, seek emergency attention.
If you note any other changes from your dog’s normal behavior, make sure to discuss these with your veterinarian. The more information your veterinarian knows, the easier it will be for them to find out what’s causing your dog’s lethargy.
Diagnostics for Lethargic Dogs
Your veterinarian’s very first step will be to discuss your pet’s history and perform a full examination. The information your veterinarian gathers will drive what diagnostics they perform next.
Common diagnostics for a dog showing lethargy include:
- Blood and urine tests to look at overall organ function
- X-rays
- Abdominal ultrasound
In puppies and unvaccinated dogs, parvovirus tests are also common for lethargic dogs.
In some cases, additional testing may be recommended. This would depend on your individual pet’s symptoms and what baseline testing shows.
Treatment for Dog Lethargy

The treatment for your dog’s lethargy will depend on the suspected cause: a dog suspected of having a bacterial infection may be given antibiotics. A dog with diabetes may be started on insulin and a special diet, while a dog with arthritis might start taking pain medication.
Your pet’s overall prognosis depends on the underlying cause. For example, an infection may improve over 10 to 14 days. Dental pain may resolve within a week or two of a professional dental cleaning. Arthritis pain may be controlled after a month or two of consistent treatments but may relapse as the arthritis worsens. Dogs with systemic health conditions like chronic kidney disease may also improve with supportive care but later decline as the condition progresses. Your veterinarian is your best source for what to expect in your pup’s individual case.
Bottom line, if you have any concerns about your dog’s behavior, including decreases in their energy level, it’s important to speak with your veterinarian. Lethargy in dogs generally has an underlying cause and shouldn’t be ignored.
Dental Treats for Dogs: 6 to Consider
- 2025-01-06T15:35:43
- Paula Fitzsimmons
According to vets, daily tooth brushing is the most important thing pet parents can do to help prevent periodontal disease in dogs. However, as many of us know first-hand, life (and uncooperative canines) can often get in the way. Here’s hope: If you’re facing the occasional skip day, dental treats for dogs could help you keep your dog’s oral health on track.
While there’s no replacement for regular brushing and professional cleaning, dog dental chews and treats can play a role in your dog’s dental care. That’s because they can help reduce the plaque and tartar accumulation that causes dental disease.
Whether you reach for them in a pinch or to supplement your dog’s regular dental hygiene routine, here’s the scoop on dog dental treats. Plus, we asked vets about what to look for in dog teeth-cleaning treats and their top-recommended picks.
Dental Treats for Dogs: How Do They Work?

With the word “treats” right there in the name, it’s easy to assume that dental treats and chews are simply dog-safe breath mints. However, they do much more than help eliminate bad doggy breath.
“Although not as effective as brushing, the mechanical or chemical action of a dental treat can help reduce the amount of plaque and calculus build up on dog teeth,” says dental hygienist Kimi Kan-Rohrer, RDHAP, BSDH, at the University of California-Davis Veterinary Medical Teaching Hospital. “This, in turn, helps reduce the development of periodontal disease,” she adds.
Dog dental treats aren’t without their limitations. Even the best dog dental chews can’t fix damaged teeth. “They can’t treat more advanced dental issues like severe periodontal disease, abscesses, or tooth decay,” says Dr. Lisa Lippman, DVM, director of Virtual Medicine at Bond Vet. “Those require professional veterinary care.”
Using dental treats for dogs in tandem with regular brushing and professional veterinary cleanings is ideal. However, it’s not always feasible, acknowledges Dr. Don Beebe, DVM, DAVDC, co-founder of Apex Veterinary Specialists in Greenwood Village, Colorado.
For example, “Some pets have a strong aversion to direct tooth contact, ” Dr. Beebe explains. “Sometimes, it is the pet owner with the limitation. They may have poor compliance due to their schedule or perhaps a physical impairment that makes toothbrushing difficult.”
Types of Dog Dental Treats

Dog dental treats come in various shapes and sizes. And you may even know them by different names. On one hand, you’ll see dental treats and dental chews for dogs. But you may also see products like rawhide sticks, bones, or chews and wonder if they can benefit your dog’s dental health.
What’s the difference between these options for dogs? Here’s a quick breakdown to help you understand what to look for.
Edible Dental Treats for Dogs
Dog dental treats are typically designed to be chewed and digested. While the formulas vary, these treats typically contain ingredients like wheat flour, gelatin, corn starch, rice, chicken, and honey. So they are safe for canine consumption.
They may also contain chemical compounds, such as delmopinol hydrochloride or hexametaphosphate, to prevent plaque or tartar accumulation. Many have vitamins and minerals (like calcium) that aid in dental health.
You may hear these edible options called either chews or treats.
Dog dental chews can take the form of sticks, bones, toothbrushes, or any shape imaginable. They usually have a tough texture to encourage chewing and gnawing because that helps remove plaque and tartar. “Dental chews for dogs with a tougher texture can offer better mechanical cleaning action,” says Dr. Lippman.
Dog dental treats are typically smaller and bite-sized. They’re often not as tough, making them a good option for dogs who have difficulty chewing. You can even use some smaller dog dental treats as a food topper.
Non-Edible Bones, Sticks, and Chews

Rawhide is an example of a non-edible chewing treat. While studies show that chewing rawhide is an effective way to reduce plaque and tartar, it can be dangerous for dogs.
Rawhide “can be a choking hazard and harder for your dog to digest,” says Dr. Amber Karwacki, DVM, a partner doctor with Heart+Paw in Philadelphia.
If you choose to give your dogs these types of chewing treats, be aware that they aren’t formulated for dental benefits, like dog dental treats are. And always supervise your dog so they don’t ingest bits of rawhide.
Vet-Approved Dental Dog Treats
All featured products are chosen at the discretion of the Great Pet Care editorial team and do not reflect a direct endorsement by the author.
We considered a variety of dental chews and treats for dogs. And these are the top picks based on recommendations (or recommended product features) from veterinarians.
Our List
- Greenies Dental Treats for Dogs
- OraVet Dental Hygiene Chews
- C.E.T. VeggieDent Chews for Dogs
- ProDen Dental Care Dental Bites
- Pedigree Dog Treats Dentastix
- Purina DentaLife Dog Dental Chews
All our recommendations are available without a prescription. However, it doesn’t hurt to check with your veterinarian to be sure the product you’re considering is a good fit for your pup.
Dental Dog Treats: What to Look For

According to veterinarians, here are some things to keep in mind when shopping around for dental treats and chews.
Look for the VOHC label
The Veterinary Oral Health Council (VOHC) is a group of veterinary dentists and scientists appointed by The American Veterinary Dental College. They review pet dental products to see if they really work to reduce plaque and tartar.
If a product meets their standards, it gets the VOHC Seal of Approval. This seal tells pet parents and veterinarians the product is effective in promoting healthier teeth in pets.
To earn this seal, manufacturers must “complete clinical trials and provide research to prove their product reduces plaque and/or calculus (tartar) by at least 15 percent,” explains Dr. Kan-Rohrer.
If a product does not bear the VOHC Seal of Approval, that doesn’t necessarily mean it’s not effective, Dr. Kan-Rohrer adds. It could be that “they just haven’t submitted for VOHC review due to cost or lack of clinical trial data,” she notes.
Find options that fit your dog
Choose canine dental chews and treats that are appropriate for your dog’s size. “That way, you can avoid the risks that come with eating them too quickly or swallowing them whole,” says Dr. Kan-Rohrer. “These include choking, esophageal obstruction, and GI obstruction,” she warns.
Also, check the label for any ingredients that may trigger an allergic response in your dog or cause other health problems. For example, if your dog has thyroid issues, avoid chews with iodine-rich ingredients.
Ingredients to avoid
Veterinarians recommend avoiding treats containing excessive refined sugar because they can contribute to weight gain or other health issues. If your pet has food allergies, you should also avoid dental treats that contain ingredients that cause an allergic reaction.
Also, steer clear of products with xylitol or fluoride because they can be toxic to dogs (and cats), adds Dr. Kan-Rohrer. Treats that are approved for dogs should not have these ingredients.
Check the texture
Texture is an important feature of good dental chews for dogs. “Dental treats should be firm on the outside and chewy on the inside,” recommends Dr. Karwacki. The combo encourages your dog to bite on the treat multiple times, which helps scrape plaque and tartar from their teeth, she notes.
6 Best Dental Treats for Dogs that Vets Recommend

Greenies Dental Treats for Dogs
The plaque and tartar fighting power of Greenies Dental Treats for Dogs comes, in part, from their tough, chewy texture. The treats also feature distinctive grooves to promote chewing and prevent dogs from swallowing large chunks.
Greenies “are designed to be easily digestible,” says Dr. Lippman. “They also contain added ingredients that freshen breath.” (Their Fresh line contains natural dried spearmint.)
Greenies dog dental treats contain added nutrients like antioxidants vitamins A and E, and minerals, including calcium, which is essential for strong teeth. Best of all, Greenies has an extensive line of specialized dental treats, including Aging Care for older dogs and Weight Management.
Highlights
- The unique design promotes chewing activity and prevents dogs from swallowing large chunks.
- They contain added vitamins (like A and E) and minerals like calcium.
- Greenies Dental Treats for Dogs carry the VOHC Seal of Acceptance.
- The Greenies line comes in a wide variety of formulas, flavors, and sizes.
Things to Consider
- Greenies offers a sweet potato flavor variety. While antioxidant-rich sweet potatoes provide important nutrients, Dr. Beebe says these starchy treats could increase the risk of cavities in some dogs. “They may be okay if the pet’s teeth are brushed regularly,” he cautions.

Oravet Dental Hygiene Chews
These are among the best dog chews for teeth because they offer dual benefits, fighting bad breath and plaque at the same time. They also contain delmopinol hydrochloride, a chemical compound used in human dentistry.
“When added to a dental treat, this molecule helps make the tooth surface more slippery,” says Dr. Beebe. That helps by making it harder for plaque and tartar to accumulate. Oravet Dental Hygiene chews come individually wrapped for freshness.
Highlights
- This dual-action chew contains delmopinol hydrochloride, a compound that helps stave off plaque and tartar buildup.
- Each chew is individually wrapped for freshness.
- They’ve earned the VOHC Seal of Acceptance.
Things to Consider
- Oravet dog dental chews don’t come in as many varieties as some competitors.
- Individual wrapping of each treat contributes to waste.

C.E.T. VeggieDent Chews for Dogs
The signature Z-shape of this plant-based chew is by design. The unique shape makes it easier for the chew to reach (and clean) more areas of the dog’s mouth.
VeggieDent chews are one of the dog dental treats Dr. Karwacki recommends to pet parents. “These chews tend to hold up to some of the tougher chewers,” she says. They’re easily digestible and contain a prebiotic to promote gastrointestinal health.
The VeggieDent line isn’t just about dental health. You’ll find options that promote joint health and cognitive ability, too. An added plus: They’re manufactured by Virbac. So your purchase contributes to the company’s Every Pet Project, which donates $2,500 to two animal charities each month.
Highlights
- The unique shape makes it easier to reach more areas of the mouth.
- VeggieDent dental chews contain a prebiotic to aid in gut health.
- Available in unique formulations that focus on joint, gut, and mental health in addition to removing plaque.
- Seal of Acceptance from the VOHC.
- Virbac runs the Every Pet Project.
Things to Consider
- C.E.T. products are not as widely available in stores as some other better-known brands, and they’re a bit pricier.

ProDen Dental Care Dental Bites
These soft, small-sized dental bites can be a good option for dogs who have difficulty chewing. Another benefit: They contain sustainably sourced Scandinavian kelp that helps prevent plaque and calculus accumulation in dogs, according to one manufacturer-funded study.
While kelp is rich in antioxidants, feeding too much of it to a dog can lead to hyperthyroidism, due to its potent iodine content.
Highlights
- Good option to consider for dogs who have difficulty chewing.
- Formulated with an antioxidant-rich form of kelp that’s been studied for its effectiveness in removing plaque and tartar.
- These dog dental chews bear the VOHC Seal of Acceptance.
- ProDen dental treats are available as bites, soft chews, and “bones”.
Things to Consider
- Excessive kelp consumption can lead to hyperthyroidism.
- ProDen products are not as easy to find at retailers as some of our other recommended products.

Pedigree Dog Treats Dentastix
The key feature of the Dentastix chew is its deeply grooved, X-shaped design. According to the manufacturer, the unique shape makes it easier to clean hard-to-reach places in your dog’s mouth.
These treats feature calcium for strong teeth and beneficial vitamins like A, D3, and B. Dentastix chews are available in beef, chicken, and bacon flavors to tempt the most discerning of canine palates. They also have a minty flavor to help combat bad breath. The Pedigree Foundation donates millions of dollars to U.S. animal shelters and rescues.
Highlights
- The unique shape allows the chew to make its way to hidden areas of the mouth.
- Contains beneficial vitamins and minerals.
- Pedigree dog dental treats are available in a variety of flavors.
- They’re easy to find at retailers and are a more cost-effective option.
- The Pedigree Foundation supports U.S. rescues and shelters.
Things to Consider
- Though they’re made in the U.S., some of their ingredients are sourced from China and other countries.
- The only Dentastix product currently assigned the VOHC Seal of Acceptance is Pedigree Dentastix Advanced.
Purina DentaLife Dog Dental Chews
These porous dental sticks are ridged to promote chewing and plaque removal in difficult-to-reach places. They come in chicken flavor, with some varieties incorporating apple, pumpkin, and blueberry flavors into the mix.
The DentaLife line offers dog dental chews that promote immune health and digestion while also removing plaque buildup. They’re manufactured by Purina, a brand that provides grants to animal shelters and helps facilitate adoptions through its Purina + Petfinder Foundation.
Highlights
- Ridges in the chew make it easier to remove plaque in hidden areas of the mouth.
- Formulated with calcium.
- The DentaLife line includes dental chews that also target immunity and digestion.
- Has the VOHC Seal of Acceptance.
- Purina products are easy to find at retailers.
- Purina supports animal shelters and helps facilitate adoptions.
Things to Consider
- Some of their dog dental chews contain honey.
Tips for Using Dog Treats for Dental Care

Supervise your dog
Dr. Karwacki encourages pet parents to observe their dogs closely when giving them dental treats, especially in the beginning. That way, they can be sure their dog is chewing it appropriately and not attempting to swallow large pieces.
Monitor calorie intake
According to the Association of American Feed Control Officials (AAFCO), dog dental treats are not complete-and-balanced foods. So they should not be used in place of your dog’s regular diet. But if you’re adding them to your dog’s daily food intake, do so sparingly as some can be high in calories.
“To avoid weight gain, reduce the pet’s food intake proportionately to the calories provided by treats,” says Dr. Beebe.
Keep in mind that your dog’s normal diet should comprise at least 90 percent of their calories. Your dog should get no more than 10 percent of their calories from treats, which includes dental treats and chews.
Watch for signs of injury
In some cases, consuming too many dog dental treats can cause serious health issues. Dr. Beebe cites the risk of dogs developing pancreatitis, especially if the treats are high in fat. “If the product is excessively dense or hard, there is also a risk of tooth or gum injury,” he notes.
Such injuries could be even more serious for dogs with fractured teeth or those recovering from oral surgery, says Dr. Beebe. “Dogs with excessive chewing behaviors could potentially irritate gum tissues.” Dr. Lippman recommends checking your dog’s gums for irritation or injury after using a new dental treat.
Always remember, even the best dog teeth-cleaning treats can never replace consistent daily brushing and professional dental cleaning for your dog. If you’re ever in doubt about giving your dog dental chews or treats or need product recommendations, check with your veterinarian. When it comes to your dog’s dental or overall health, it’s always better to be safe than sorry.
Edema in Dogs
- 2024-12-30T20:52:13
- Natalie Marks, DVM
When I was pregnant with my third child, I noticed that my swollen ankles would retain an imprint of my fingers if I pressed them. Thankfully, this condition (called pitting edema) wasn’t a significant concern. However, this type of swelling is not just limited to humans or pregnancies. Edema in dogs can be far more serious.
Dogs can develop edema around the body. The condition can range from mild to severe and even life-threatening, depending on the cause. So let’s explore what edema in dogs is, its causes, symptoms, diagnosis, and treatment. We’ll cover how to reduce edema in dogs and how pet parents can help their furry friends.
What is Edema in Dogs?
While people often use edema and swelling interchangeably, let’s understand the relationship between these two terms.
Swelling refers to any abnormal buildup of fluid. However, edema in dogs is a specific type of swelling caused by fluid accumulation in the tissues between the body’s cells. It indicates a fluid imbalance.
Either too much fluid escapes the blood vessels into the tissues, or too much fluid remains trapped in tissue without returning to the bloodstream.
Causes of Edema in Dogs

The causes of edema in dogs can vary widely, depending on the affected area. Here are some common categories:
- Cerebral Edema: Swelling in the brain due to traumatic injury, severe infections, diabetes, or electrolyte imbalances.
- Pulmonary Edema in Dogs: Fluid buildup in the lungs leading to coughing and difficulty breathing. Prompt treatment can improve outcomes. If untreated, it can be life-threatening.
- Abdominal Edema (Ascites): Caused by liver failure, heart failure, or kidney failure, leading to fluid accumulation in the abdominal cavity (swollen belly).
- Localized Edema: Often a result of trauma, such as a laceration after an altercation with an animal or a swollen incision after surgery.
- Peripheral Edema: Commonly affects the lower legs, ankles, or paws. Often called leg edema in dogs. Occurs due to conditions like vasculitis, drainage blockages, or low levels of albumin.
- Facial Edema in Dogs: Often linked to allergic reactions (to things like foods, medications, or insect bites), tooth root infections, or tumors.
- Corneal Edema in Dogs: Swelling in the cornea causing cloudiness or vision issues.
- Peripheral Edema: One of the more common forms of edema, this swelling occurs in the lower legs, ankles, or paws of dogs. This can happen for several reasons, including vasculitis (inflammation of the blood vessels), a blockage of the drainage system, and a lower level of an essential body protein called albumin. [1]
In addition, some cancers like lymphoma and mast cell tumors, can trigger edema anywhere in a dog’s body by disrupting the normal fluid drainage in the region of the cancer. [2]
Signs of Edema in Dogs

Some forms of swelling are pretty obvious, like puffiness in the face after a bee sting. However, not every form of edema is immediately visible to the naked eye.
For example, cases of pulmonary edema in the lungs or cerebral edema in the brain may be more challenging to spot. In these cases, we look for more vague signs suggesting internal edema may be present.
The sooner you can recognize signs of edema in dogs, the sooner you can get your pet the care they need. So here’s a guide to key signs to watch out for, and what they can mean.
- Visible swelling: First and foremost, an essential sign of edema in dogs is the swelling itself. This can appear as obvious puffiness in areas like the face, legs, or belly. Facial swelling is common when there has been trauma, tooth root infections, allergic reactions, and even cancerous tumors.
- Change in appetite: This could be anything from a decrease in the total amount of food eaten to a change in the eating pattern, also known as dysrexia.
- Change in energy level: Dogs may seem tired, not interested in normal daily activities, or less playful.
- Weight gain: Some dogs with edema gain a significant amount of weight rapidly with no change in appetite.
- Pain: Dogs with edema may show unexplained whining, restlessness, and trouble lying down or sleeping.
- Seizures: These can be most closely associated with edema of the brain tissue in dogs. Other signs of cerebral edema in dogs include disorientation and other neurological changes.
- Trouble breathing: Coughing and difficulty breathing could indicate pulmonary edema in dogs (swelling in the lungs/airways). These signs could be life-threatening and require immediate attention.
Edema in Dogs Diagnosis

Remember, edema in dogs is a sign of an underlying disease. Your veterinarian’s first priority will be to confirm if your dog has edema and where. Then, they’ll investigate the underlying cause. Here’s how that typically works
History and Physical Exam: Your vet will ask detailed questions about your dog’s physical symptoms and when you first noticed them. They’ll also ask about any recent injuries, medications your dog takes, previous diseases, and changes in behavior.
Lab Work: If your vet suspects edema, they typically recommend further diagnostic testing. Blood and urine tests can help identify infections, inflammation, or organ dysfunction.
Imaging: Your vet may also recommend imaging to get a clearer picture of potential edema in dogs. X-rays and ultrasounds can detect fluid accumulation in areas like the lungs or abdomen. Advanced imaging like CT or MRI may be needed for conditions like cerebral edema.
How to Treat Edema in Dogs

When veterinarians diagnose edema in dogs, there are three main goals for treatment:
- Identify and treat the underlying cause
- Remove the fluid to resolve the clinical signs
- Restore fluid balance in the body
Understanding the underlying cause of edema in dogs plays a big role in effective treatment. Depending on that cause, your veterinarian may hose one or more of the following treatments:
- Diuretics: Medications to remove fluid in cases like pulmonary edema
- Manual Removal: Fluid may be drained via needle for abdominal edema
- Anti-inflammatories and antibiotics: Used for infections or inflammatory causes of edema
Long-term management relies on some of the above strategies but may also require dietary changes, nutritional supplements, or surgical corrections in some cases of organ failure.
Dog Edema Cost and Prognosis
The cost and prognosis for edema in dogs vary widely based on the underlying cause and severity. For instance, the survival rate for pulmonary edema in dogs improves significantly with early intervention. Chronic conditions like heart or kidney disease may require ongoing management.
How to Help a Dog with Edema

It’s important to note that even if your dog’s edema resolves, that doesn’t mean your worries are over. Removing the fluid is typically just part of the treatment plan for whatever caused the edema in the first place.
Helping a dog with edema involves both veterinary treatment and home care. Many dogs with edema have significant underlying diseases that require lifelong therapy. And even minor cases of swelling, such as bee stings, require follow-up care.
To ensure the best outcome for your pet, keep these tips in mind.
Follow your vet’s treatment plan and recommendations – Administer medications as prescribed and maintain regular follow-ups to help manage any underlying causes of edema.
Monitor your dog closely – Watch for recurrence of swelling, trouble breathing, or other concerning signs. Alert your veterinary team as quickly as possible if you notice any signs that your dog’s edema has returned.
Feed your dog a vet-recommended diet – If your vet recommends specific dietary adjustments to help support your pet’s recovery, be sure to incorporate them. Diet can play an important part in helping prevent recurrence.
Keep your dog comfortable – Create a comfortable resting area for your dog and minimize any stress that could impact their health or wellness.
Edema in dogs can be a challenging condition for both pets and their owners. By understanding the signs, causes, and treatment options, you can act quickly and ensure your dog receives the best care possible.
Always consult your veterinarian if you notice any signs of edema, as early intervention is key to a better prognosis and your dog’s overall health.
References
- Whelchel, Bradley D et al. “Retrospective evaluation of the etiology and clinical characteristics of peripheral edema in dogs.” Journal of veterinary internal medicine vol. 37,5 (2023): 1725-1737. doi:10.1111/jvim.16815
- Kim, Sangho, and Arata Matsuyama. “Canine mast cell tumors: When to worry about aggressive behavior pre-surgically.” The Canadian veterinary journal = La revue veterinaire canadienne vol. 63,12 (2022): 1261-1263.
Are Toads Poisonous to Dogs?
- 2024-12-20T15:41:35
- Elizabeth Claire Alberts
Most dogs love chasing balls, sticks, cars, and even small animals — so, it makes sense that dogs would happily run after toads as well.
It’s completely normal for dogs to want to chase a toad, says Dr. Anna Kaufman, a veterinarian at Bond Vet in New York. “Dogs are naturally curious, especially with small, jumpy critters like toads,” she says. “Their instinct to chase can be pretty strong — after all, a bouncing toad is like a real-life squeaky toy!”
While your dog’s instincts are natural, it’s best to supervise your dog’s outdoor activities closely, Dr. Kaufman says, especially if you know you’re in an area where toads are common. This is because many toads are poisonous and can cause your dog to get sick. In some cases, biting or ingesting a toad can threaten your dog’s life.
To keep your dog safe, here’s what pet parents should know about toads and what to do if your dog grabs one.
Are Toads Poisonous to Dogs?

Yes, many toads are poisonous to dogs, Dr. Kaufman says. However, some toads are more dangerous to dogs than others. If your dog does come into contact with a particularly poisonous species, their life may be at risk.
Other toads won’t threaten your dog’s life, but the toads may still have “toxins in their skin that are dangerous if ingested,” Dr. Kaufman says.
The extent to which a toad can harm your dog can also depend on the amount of exposure. “Oral exposure to toads can be very serious, even fatal in some cases, depending on the type of toad and how much contact your dog had,” Dr. Kaufman says. “For highly toxic toads, even a lick can cause severe symptoms. With less toxic toads, it might cause some irritation but usually isn’t life-threatening.”
Toads Poisonous to Dogs
So, which toads should pet parents be on the lookout for? Two of the most dangerous toads to dogs are the cane toad and the Colorado River toad. “These toads have powerful toxins that can be life-threatening to dogs if ingested, so it’s essential to keep your pup away from them,” Dr. Kaufman says.
The cane toad — also known as the marine toad, giant toad or bufo toad — is a large toad with warty and brown mottled skin. This toad is native to South America, but it is also found in south or central Florida in the U.S. The toad was also introduced to Australia in the 1930s in an attempt to control beetles on sugar cane fields, but the toads spread across Australia and it is now considered an invasive species.
The Colorado River toad — also known as the Sonoran Desert toad — is a large toad with greenish-grey coloring on its topside and white on its underside. Its native range is through a small part of northern Mexico, as well as part of New Mexico, Arizona, and California in the United States.
Other types of toads may cause a condition called toad poisoning in dogs, but they are generally not a threat to dogs’ lives.
Toad Poisoning in Dogs Symptoms

When a dog bites or ingests a toad, they can experience a condition known as toad poisoning or toxicosis. However, this condition is only serious or life-threatening if it involves a species like the cane toad or the Colorado River toad.
According to Dr. Kaufman, common signs of toad poisoning in dogs may include:
- Drooling
- Vomiting
- Pawing at the mouth
- Foaming at the mouth
More serious symptoms may include:
- Weakness
- Tremors
- Difficulty breathing
- Seizures
Toad Poisoning in Dogs Treatment
If you see your dog with a toad or notice any signs of toad poisoning, rinse out your dog’s mouth in a careful manner, making sure they don’t inhale water containing the toad toxin, Dr. Kaufman says. You should also contact your vet or an emergency clinic immediately. “Acting fast can make a huge difference,” she says.
For potentially toxic toad exposures, a trip to the emergency vet is wise, Dr. Kaufman says, and quick treatment is key to preventing severe symptoms or complications.
At the clinic, your veterinarian will assess your dog and try to help them recover from toad poisoning.
“Your vet will likely flush out any remaining toxins and monitor your dog’s heart and neurological signs,” Dr. Kaufman says. “Depending on the severity, they may administer medications and supportive care to manage symptoms. Recovery varies but can take a few hours to a few days, and most dogs do well with prompt treatment.”
Prevention

“The best prevention is to supervise your dog outdoors, especially at dawn and dusk when toads are most active,” Dr. Kaufman says. “If toads are common in your area, consider leash-walking your dog to keep them close and out of trouble.”
While your dog’s health and safety is the most important thing, it’s also helpful for dogs to leave toads alone to help maintain local ecosystems, Dr. Kaufman says.
“Toads are beneficial to the environment, helping control insect populations,” Dr. Kaufman says, “so let’s give them space and keep our pups safe at the same time!”.
Enzymatic Toothpaste for Dogs: What it is and Products to Try
- 2024-11-30T22:32:40
- Liz McCalley, DVM, CCRT
Effective dental care is an essential part of keeping dogs happy and healthy. However, it can prove a tricky task, even for the most diligent pet parents. Research shows that up to 80 percent of dogs over the age of 2 years have periodontal (gum) disease (1). But before you throw in the towel (or the doggy toothbrush), if you’re looking for an easier way to promote your pup’s oral health, enzymatic toothpaste for dogs could be the key.
This specialized toothpaste is designed to make cleaning your dog’s teeth easier and more effective than standard dog toothpaste. Plus, it helps combat common oral health issues like plaque, tartar buildup, and bad breath.
Whether you’re new to canine dental care or looking for a better solution, enzymatic toothpaste is worth considering. Let’s explore what it is, how it works, and which products are vet-approved for optimal doggy dental health.
What Is Enzymatic Toothpaste for Dogs?

Enzymatic toothpaste for dogs is a type of toothpaste that contains enzymes — proteins that speed up chemical reactions. In dog toothpaste, these enzymes help break down food particles, sugars, and bacteria in your dog’s mouth, making it harder for plaque to form.
Unlike human toothpaste, enzymatic toothpaste for dogs is safe to swallow. In fact, many options come in flavors like chicken or peanut butter to appeal to dogs’ palates. This makes it easier for pet parents to establish a regular brushing routine without the struggle.
Enzyme Toothpaste for Dogs: How It Works

While traditional canine toothpastes often rely on abrasive ingredients or detergents to clean teeth, enzymatic toothpaste uses a different approach. The enzymes work by targeting the root cause of dental disease: bacteria.
Some of the most common enzymes found in enzymatic toothpaste for dogs include:
- Glucose oxidase – Produces hydrogen peroxide, which helps reduce bacterial populations
- Lactoperoxidase – Inhibits bacterial growth
- Amyloglucosidase – Breaks down complex sugars into simpler components, preventing plaque buildup
When these enzymes are used alone or in combination, they create an environment where bacteria struggle to thrive or attach to tooth surfaces, improving oral health over time.
This means that even if you aren’t able to scrub the bacteria from your dog’s teeth through brushing, the enzymatic activity of the toothpaste will still help to kill disease-causing bacteria (2).
Benefits of Canine Enzymatic Toothpaste
Adding enzymatic toothpaste to your dog’s dental care routine offers numerous benefits:
- Combats plaque and tartar – Prevents the buildup of harmful substances that lead to periodontal disease
- Fights bad breath – Targets the bacteria that cause unpleasant odors
- Reduces the risk of tooth decay – Protects your dog’s teeth from cavities
- Supports overall health – Poor dental hygiene is linked to issues like heart, liver and kidney disease in dogs
- More effective than other products – Enzymatic toothpaste is often more efficient at cleaning than certain powders, gels, or rinses because it actively reduces plaque accumulation, which is the cause of periodontal disease
Best Enzymatic Toothpaste for Dogs: 5 Picks Vets Recommend

Virbac C.E.T. Enzymatic Dog Toothpaste

Highlights
This toothpaste is a gold standard for dog dental care and is the toothpaste brand most recommended by board-certified veterinary dentists. It’s formulated with a combination of glucose oxidase and lactoperoxidase, making it highly effective at breaking down plaque. Plus, it comes in a variety of enticing flavors like poultry and vanilla-mint to appeal to even the pickiest pups.
Things to Consider
Certain flavors, like beef and chicken, may upset your dog’s stomach if they have a food allergy.
Oratene Brushless Enzymatic Gel

Highlights
Ideal for dogs with sensitive gums or pets who don’t tolerate brushing, this gel works without the need for vigorous scrubbing. Simply apply it to your dog’s teeth, and the enzymes will do the work.
Things to Consider
Works best when applied daily.
Enzadent Enzymatic Toothpaste

Highlights
Contains zinc in addition to enzymes for added activity against plaque and bacteria. Comes complete with a fingerbrush cap so it’s perfect to take on the road. Its poultry flavor is highly palatable to most dogs.
Things to Consider
Contains chicken.
Buster Toothpaste with Enzymes

Highlights
In addition to containing enzymatic ingredients, this toothpaste contains chlorhexidine, a highly effective antibacterial agent. This toothpaste is best suited for dogs with severe gingivitis.
Things to Consider
Because Buster toothpaste contains chlorhexidine, it is not recommended to use this product long term, as it may lead to bacterial resistance to the active ingredient and can eventually lead to increased tartar accumulation. Ask your veterinarian if this toothpaste is right for your dog and how long they would recommend its use.
Petsmile Professional Dog Toothpaste
Highlights
The only Veterinary Oral Health Council-approved dog toothpaste. While not technically enzymatic, it uses calcium peroxide to stop plaque formation on tooth surfaces.
Things to Consider
More expensive than other options but may be worth it for its proven efficacy.
Enzyme Toothpaste for Dogs: What to Look For

When shopping for enzymatic toothpaste for your dog, consider the following:
- Ingredients: Look for products with enzymes like glucose oxidase or lactoperoxidase. Avoid harmful additives like xylitol, which is toxic to dogs.
- Flavor: Choose a flavor your dog loves in order to make brushing easier. Ask your veterinarian for recommendations if your dog has any food allergies or food sensitivities.
- VOHC approval: Products with the Veterinary Oral Health Council seal have been tested for efficacy.
- Compatibility: Ensure the toothpaste is safe for daily use and appropriate for your dog’s specific needs.
Tips for Using Dog Enzymatic Toothpaste

To get the most out of enzymatic toothpaste, follow these tips:
- Start slowly: Introduce the toothpaste gradually to let your dog get used to the taste and texture.
- Use a dog toothbrush: While applying the enzymatic toothpaste alone without brushing will help to reduce plaque and gingivitis, it will not be nearly as effective as when combined with brushing. A soft-bristled brush designed for dogs will be gentler on their gums.
- Brush regularly: Aim for at least 2-3 times per week for optimal results. If your dog already has gum disease, daily brushing is imperative.
- Check for sensitivities: When using any new oral care product, ensure it is well tolerated by your dog and does not cause any vomiting or diarrhea.
- Always use dog-safe toothpaste: Never use human toothpaste, as it can contain ingredients harmful to dogs.
Enzymatic toothpaste is a game-changer for canine dental care. By incorporating it into your dog’s routine, you can improve their oral health, prevent serious diseases, and keep their tail wagging for years to come.
For the best results, always combine home dental care with regular veterinary oral exams. Your veterinarian can give you the best advice on what toothpaste and other oral care products are most appropriate for your dog.
References
- Barbosa, E., et al. “Strategies to Improve the Home Care of Periodontal Disease in Dogs: A Systematic Review.” Research in Veterinary Science, vol. 154, 1 Jan. 2023, pp. 8–14, doi:10.1016/j.rvsc.2022.10.025
- Watanabe, Kazuhiro et al. “Inhibitory effect for proliferation of oral bacteria in dogs by tooth brushing and application of toothpaste.” The Journal of veterinary medical science vol. 78,7 (2016): 1205-8. doi:10.1292/jvms.15-0277
8 Fungal Infections in Dogs You Should Know About
- 2024-11-22T20:39:20
- Rhiannon Koehler, DVM, MPH
When you hear that your dog has an infection, you’re most likely thinking of a bacterial or viral infection. However, viruses and bacteria aren’t the only pathogens that can affect our pets. Dogs can also contract fungal infections.
While most fungal infections in dogs are restricted to the skin or ears and are easily treated, some fungal infections affect the dog systemically and can be life-threatening. Learn about fungal infections in dogs and how they’re treated.
How Do Dogs Get Fungal Infections?
Dog fungal infections are caused by fungi, which are living organisms that spread in the environment by producing spores. Most commonly, fungi live in the soil. The spores that infect dogs are microscopic.
Fungal infections on the skin, like ringworm, usually pass directly through skin contact or contaminated surfaces. Most of the fungi that infect internal organs are inhaled, but they can also be ingested or enter the dog’s system through an open wound.
Dogs who spend more time outside, like hunting dogs, may be at an increased risk of contracting a systemic fungal infection. Most of the systemic fungal infections, like histoplasmosis and blastomycosis, are not contagious between dogs.
Some canine fungal infections are more prevalent in specific geographic locations. For example, histoplasmosis and blastomycosis are more common in the Midwest United States while coccidioidomycosis is more prevalent in the Southwest United States.
Dog Fungal Infection Symptoms
The symptoms of a dog fungal infection depend on the type of fungus and which part of the dog is affected.
For example, skin infections like dermatophytosis (ringworm) might cause scaly pink lesions on the skin and hair loss. A Malassezia infection of the ear might cause dark brown discharge, itchiness, and a foul odor from the ear. Blastomycosis in the lungs might cause coughing, while histoplasmosis in the gastrointestinal tract might cause diarrhea.
Symptoms of a fungal infection in dogs can include:
- Fur loss
- Scaly lesions on the skin
- Coughing
- Loss of appetite
- Itchiness
- Difficulty breathing, coughing, or congestion
- Vomiting
- Diarrhea
- Fever
- Nasal discharge
- Dark debris in the ear
8 Types of Fungal Infections in Dogs

Dogs can contract a variety of fungal infections. Here, we’ll cover eight important canine fungal infections.
Dermatophytosis (Ringworm)
Type: Skin
You may be surprised to hear that ringworm isn’t actually a worm at all — it’s a fungus! Ringworm is a common dog fungal skin infection. The fungus passes directly from animal to animal via physical contact. Infection from contaminated environments, such as an uninfected dog lying in the bed of an infected dog, is also possible.
Dogs with ringworm develop scaly areas of hair loss. The skin may be itchy, though this isn’t always the case.
Your veterinarian should give you instructions on how to clean the environment while your pet is undergoing ringworm treatment. Treatment usually entails both topical therapies and oral medications. Topical therapy can include antifungal baths like lime sulfur dips, shampoos with antifungals, and leave-on creams. The oral antifungal drug of choice for dogs with ringworm is terbinafine.
Ringworm can pass from a pet to a person, so it’s important to regularly wash your hands and decontaminate the environment if your pet has ringworm. If you have a lesion that you suspect is ringworm, it’s best to consult with a medical professional.
Malassezia
Type: Skin
Malassezia dermatitis is caused by overgrowth of Malassezia yeast, which is a normal yeast on the skin. Most commonly, this occurs in dogs who have an abnormal skin barrier, such as dogs with allergic skin disease.
Dogs with a Malassezia infection will usually have very itchy skin with areas of redness, thickened skin, and/or hair loss. The coat may be oily, and the pet parent may notice a yeasty smell.
Malassezia is also responsible for most dog fungal ear infections and dog paw fungal infections. When a dog has a yeasty ear infection, the ear will often be quite itchy, red, and have dark debris inside. On the paws, the nailbeds are commonly affected, and a dark discoloration of the nails may be noted.
Treatment may include topical antifungals like shampoos or creams and systemic oral drugs, like terbinafine. Because most dogs who get yeast skin infections have an underlying skin condition, it’s important to manage any underlying factors to prevent recurrence.
Malassezia is not usually considered zoonotic, or able to pass from animals to people. However, caution should be used if there are immunocompromised individuals in the home.
Histoplasmosis
Type: Generalized/systemic, respiratory, gastrointestinal
Histoplasmosis is a fungal disease that’s more common in young adult dogs, especially sporting (hunting) breeds. The fungus is typically inhaled by a dog nosing around in the soil. Bat and bird feces may contribute to soil contamination. Histoplasmosis can remain isolated to the lungs or gastrointestinal tract, or it can spread throughout the body.
Dogs may have general signs like lethargy, weight loss, and appetite loss. If the lungs are affected, pet parents may notice difficulty breathing and coughing. Dogs who have histoplasmosis affecting their gastrointestinal tract usually have severe diarrhea and weight loss. In some cases, histoplasmosis can affect the eyes and/or brain, causing changes to vision and neurologic signs like seizures or an abnormal gait.
For mild to moderate histoplasmosis that remains in either the lungs or gastrointestinal tract, oral antifungal medications like itraconazole or fluconazole may be used. Treatment with oral medications lasts at least four to six months. Dogs who are very sick may benefit from intravenous amphotericin B. Some dogs, especially those with lung involvement, may benefit from a short course of steroids.
Dogs who have histoplasmosis restricted to their lungs are more likely to have a positive outcome than dogs who have histoplasmosis in their gastrointestinal tract or elsewhere in the body.
Histoplasmosis does not spread from pets to people, but people can become infected with histoplasmosis from soil.
Blastomycosis
Type: Generalized/systemic or respiratory
Blastomycosis is contracted by inhaling fungal spores from soil. Dogs who roam outdoors and live close to water are at an increased risk of contracting blastomycosis.
Symptoms of blastomycosis in dogs include loss of appetite, weight loss, cough, difficulty breathing, exercise intolerance, changes to the eyes and vision, and limping. In some cases, dogs can develop neurologic signs like seizures, drunken gait, and walking in circles. The lymph nodes may be enlarged.
Out of the oral antifungals, itraconazole is the treatment of choice for blastomycosis. Fluconazole is also an option for dogs. In severe cases or cases with neurologic signs, intravenous amphotericin B may be recommended. Steroids may be recommended short-term for dogs with difficulty breathing.
Most dogs will achieve a cure with appropriate treatment, but prognosis is worse if blastomycosis has spread throughout the body. It’s also possible for dogs to experience recurrence of blastomycosis after antifungal therapy is stopped.
The disease is not transmitted from infectious dogs to people through the air. Humans can get blastomycosis from a needle stick injury, but this is more of a risk for veterinary staff than pet parents.
Aspergillosis
Type: Nasal/respiratory or generalized/systemic
Most commonly, aspergillosis is inhaled and causes a nasal infection. In some cases, however, the fungus can disseminate through the bloodstream to other parts of the body.
In dogs who have nasal aspergillosis, signs will include nasal discharge, sneezing, and bleeding from the nose. If aspergillosis has spread systemically, the dog may be lethargic, experience loss of appetite, and potentially spinal pain and weakness in limbs.
For nasal aspergillosis, treatment is to infuse intranasal clotrimazole endoscopically. For systemic aspergillosis, antifungal voriconazole is the antifungal of choice. Treatment may last for months. In some cases, antifungal treatment is lifelong.
Aspergillosis does not spread from dogs to people.
Cryptococcosis
Type: Generalized/systemic
Dogs usually contract cryptococcosis by inhaling the spores. The spores will then disseminate throughout the body in the dog’s bloodstream. Pigeon droppings are known to harbor this fungus.
Although cryptococcosis more commonly causes inflammation in the nose and sinuses (rhinosinusitis) in cats, this fungus tends to affect dogs more systemically.
Symptoms of cryptococcosis in dogs can include changes to their eyes and vision, lethargy, loss of appetite, skin masses and sores, changes to temperament, seizures, and circling. They can develop symptoms associated with the nose, like sneezing and discharge, but this is much less common in dogs than in cats.
Dogs are usually treated long-term with oral antifungals like fluconazole or itraconazole. In some cases, intravenous amphotericin B may be recommended. If large masses are present, surgical removal may be recommended. In dogs with a lot of nervous system signs, steroids may be recommended to reduce inflammation. Treatment may last for months to over a year.
The prognosis is guarded for dogs with systemic disease, especially if they have neurologic signs like seizures, blindness, or a wobbly gait.
Cryptococcosis cannot pass from your dog to you. Humans can get cryptococcosis from inhaling the spores in the air, much like our dogs do.
Coccidioidomycosis
Type: Respiratory or generalized/systemic
Coccidioidomycosis usually develops in dogs who inhale the spores from the environment. Infection may remain within the respiratory tract, or it may spread throughout the body, including to the brain and bones.
Symptoms of this fungal infection in dogs include cough, respiratory distress, loss of appetite, weight loss, lethargy, limping, skin masses, vision loss, seizures, and drunken gait. Some dogs can develop heart failure.
Treatment usually includes oral antifungals like fluconazole, itraconazole, or ketoconazole. In some cases, intravenous amphotericin B may be recommended. Dogs who have the disease limited to their lungs may have a good outcome. Prognosis is poorer for full recovery if the disease has spread to the bones and/or brain.
While there haven’t been reports of coccidioidomycosis spreading from dogs to people, there have been reports of the disease spreading to a person via cat bite.
Sporotrichosis
Type: Skin
Dogs usually get sporotrichosis when the fungus enters through a puncture wound.
In dogs, sporotrichosis is more likely to affect the skin, while cats can also develop a disseminated form that spreads throughout the body. In some cases, it can affect both the skin and lymph nodes.
Symptoms include mass-like or sore-like lesions on the skin with draining tracts. The dog is often lethargic and has a poor appetite. Lymph nodes may be enlarged.
Treatment for sporotrichosis in dogs includes an oral antifungal like itraconazole or fluconazole. Treatment usually lasts for at least 30 days after the signs have resolved.
While cat-to-human transmission is considered possible, dog-to-human transmission is unlikely or rare.
| Type of Fungal Infection | Nasal / Respiratory | Gastrointestinal | Skin | Generalized/Systemic | Zoonotic Risk |
| Dermatophytosis (Ringworm) | X | X | |||
| Malassezia | X | ||||
| Histoplasmosis | X | X | X | ||
| Blastomycosis | X | X | |||
| Aspergillosis | X | X | |||
| Cryptococcosis | X | ||||
| Coccidioidomycosis | X | X | |||
| Sporotrichosis | X | Rare |
How to Treat Fungal Infections in Dogs
The specific treatment for a dog fungal infection depends on the type of fungus.
Generally speaking, most fungal infections in dogs are treated with one or more of the following treatments:
- Topical creams like miconazole
- Antifungal baths
- Antifungal wipes
- Oral antifungal medications like itraconazole or terbinafine
Some fungal infections, particularly ones that are affecting the lungs or parts of the nervous system (like the brain) may require hospitalization. In some cases, intravenous antifungal medications like amphotericin B are recommended.
Many systemic fungal infections require months of treatment. In some cases, treatment is lifelong.
Antifungal Medications for Dogs
Veterinarians have a range of options when it comes to antifungal medications for dogs. These can include oral antifungal medications, topical medications, antifungal shampoos, and more.
Itraconazole: This is an oral antifungal that’s used for a lot of systemic fungal infections, like blastomycosis or histoplasmosis. Use in dogs is off label.
Fluconazole: This oral antifungal is often used off-label for systemic fungal infections.
Terbinafine: This oral antifungal is often used off-label for ringworm and Malassezia infections. It is sometimes used for systemic fungal infections, as well.
Miconazole cream: Miconazole is often applied directly to ringworm lesions.
TrizUltra + Keto Solution: This ear flush contains an antifungal that may be useful for fungal ear infections.
MiconaHex+Triz Shampoo: This shampoo can help with both bacterial and fungal skin infections.
Duoxo S3 Pyo Shampoo: This shampoo is also useful for bacterial and fungal skin infections.
How to Prevent Fungal Infections in Dogs
Pet parents should familiarize themselves with the fungal infections that can affect their dog in their area. Consider restricting your dog’s ability to sniff around in moist soil or near pigeon droppings.
Pet parents can also monitor their dog’s skin by practicing regular grooming. Make sure to check the skin, ears, and nails for any abnormalities when you bathe your pet or trim their nails.
Parasite prevention is important for skin health. Dogs who have skin parasites like fleas may be more likely to develop a yeasty skin infection.
Lastly, keep up on your pet’s health care! Your veterinarian may be able to detect any changes to your pet’s health before you can. They can also help you to manage underlying conditions, like allergic skin disease, that can contribute to fungal skin infections in dogs.
Acid Reflux in Dogs
- 2024-10-30T02:36:43
- Natalie Marks, DVM
In humans, heartburn and that uncomfortable “gurpy” feeling (somewhere between a gag and a burp) are often signs of acid reflux. I learned this firsthand when my doctor diagnosed me with acid reflux, also known as gastroesophageal reflux disorder (GERD). Unfortunately, this condition isn’t exclusive to humans. Acid reflux in dogs could be the source of your dog’s painful tummy troubles, too.
While acid reflux is often manageable — for both people and pups — it’s important to recognize how this condition affects your dog so you can ensure their comfort and well-being.
Let’s take a closer look at what causes acid reflux in dogs, the symptoms to watch for, and how to prevent or manage it.
What is Acid Reflux in Dogs?

Acid reflux occurs when gastric fluids (stomach acid) flow backward into the esophagus. The esophagus normally carries foods and liquids from the mouth to the stomach. In normal dog digestion, a valve called the lower esophageal sphincter (LES) prevents the stomach acid in dogs from flowing in reverse. However, in dogs with acid reflux, this valve relaxes, allowing stomach acid to backflow into the esophagus, causing irritation, inflammation, and significant discomfort.
Just like in humans, some dogs are more likely to develop acid reflux than others. So I always alert my clients to the risk factors that can increase the chances of developing the condition.
Acid reflux is particularly common in puppies and younger dogs because their LES is not yet fully developed.
Brachycephalic dogs (breeds with flat faces and short noses) also face greater risk due to their shorter esophagus and tendency to develop hiatal hernias. These high-risk breeds include:
- Pugs
- Bulldogs
- French Bulldogs
- Boston Terriers
- Boxers
- Pekingese
What Causes Reflux Disease in Dogs?

Understanding the causes of acid reflux in dogs can play an important role in preventing or managing the disease.
In some cases, you may be able to control or mitigate risk factors that could cause acid reflux. But even when you can’t (e.g., congenital causes or those that require surgical intervention), awareness may help you get your dog the care they need faster.
Common causes of acid reflux in dogs include:
- Diet and eating habits: Dogs that eat large meals too quickly and regurgitate their food are more likely to develop acid reflux.
- Foreign objects: If something gets stuck in the back of a dog’s throat or esophagus, the obstacle can prevent food from reaching the stomach. This may trigger regurgitation and acid reflux.
- Medications: Some drugs, like antibiotics and anti-inflammatory medications, can relax the LES. This makes it easier for gastric fluids to flow backward into the esophagus, causing acid reflux. Medications can also irritate the esophagus if your dog doesn’t drink enough water to wash down pills or tablets.
- Hiatal hernia: This happens when part of a dog’s stomach (and sometimes esophagus) protrudes through the layer of muscle that separates the abdomen from the chest. This can cause regurgitation and increase the risk of acid reflux.
- Chronic vomiting: Some dogs with chronic pancreatitis and liver or kidney disease experience ongoing vomiting, which can lead to chronic esophagitis.
- Obesity: Carrying extra weight can put added pressure on the abdomen, increasing the risk of acid reflux.
The Symptoms of Acid Reflux in Dogs

Any dog can develop acid reflux regardless of their risk level. That’s why it’s so important for pet parents to learn about acid reflux symptoms in dogs.
The earlier you can recognize acid reflux or GERD in dogs symptoms, the sooner you can alert your veterinarian. And the more detail you can provide, the more likely your vet will be able to diagnose and treat your dog effectively.
Here are some dog reflux symptoms to watch out for:
- Reduced appetite: Eating can be uncomfortable for dogs with acid reflux. So dogs with the condition may show less interest in food.
- Weight loss: Dogs with extreme inappetence, especially over an extended time period, will most likely lose weight, as well.
- Lip-licking and swallowing: Some dogs may demonstrate excessive lip-licking, empty swallowing, and even appear to lick the air. While we often see this in dogs experiencing nausea or dog indigestion, it can also indicate inflammation in the esophagus.
- Painful posture: Watch for general signs of pain, though this may depend on how severe the acid reflux is. Behaviors could include pacing, trouble resting, excessive vocalization, or even “prayer position” stretching, which looks like a downward dog stretch in yoga.
- Regurgitation: Another common finding in dogs with acid reflux is regurgitation after eating. Remember, regurgitation in dogs differs from vomiting. When dogs vomit, the food they’ve eaten has already reached their stomach and is forcefully brought back up. Canine regurgitation happens when food comes back up from the esophagus.
- Coughing: Dogs with frequent bouts of acid reflux can develop throat irritation, causing a hoarse, dry, spastic cough.
- Change in bark: This is one of the more specific signs of acid reflux in dogs. Throat and airway irritation can also affect canine vocal cords, resulting in a high-pitched, hoarse bark.
How to Diagnose Canine Acid Reflux

To diagnose acid reflux, your veterinarian will start by taking a thorough history. You can help by providing a detailed account of:
- your dog’s symptoms
- when the symptoms began
- your dog’s diet (including any treats or table food)
- any medications or supplements your dog is taking
- any other behaviors that seem out of the ordinary
Your veterinarian will then conduct a physical exam, possibly followed by diagnostic tests. Bloodwork and a urinalysis can help rule out other conditions with similar symptoms, such as liver, kidney, or pancreas disease. Your vet may also conduct a fecal exam to rule out parasites.
The next important diagnostic test is endoscopy. Your veterinarian will insert a small tube with a camera into your dog’s mouth, esophagus, and stomach. This will allow them to inspect the back of the throat, the lining of the esophagus (for ulcers, strictures, or foreign objects), and the stomach lining.
This test requires anesthesia. In some cases, your vet will also recommend preventative meds to minimize acid reflux during the procedure.
Treatment for Dog Acid Reflux

Thankfully, most dogs that receive treatment for acid reflux improve significantly and quickly. In many cases, a combination of medication, dietary changes, and nutritional supplements can help reduce symptoms and prevent recurrence.
Medications for acid reflux in dogs
One of the most common starting points for dog reflux treatment is antacid medication. Your veterinarian may prescribe a dog-safe antacid, such as famotidine, cimetidine, or omeprazole. These work by helping reduce the amount of acid in a dog’s stomach. While acid reflux may still occur, it’s often less damaging to the esophagus and less painful to the dog.

A second group of medications used to treat acid reflux in dogs are those that increase the muscle tone of the LES. This reduces the likelihood that stomach acid will travel backward into the esophagus. For this, your vet may prescribe cisapride or metoclopramide.


Finally, the last medication prescribed is sucralfate (also available under the brand name Carafate). This medication can help protect the lining of the esophagus, reducing the likelihood of ulcers and inflammation.
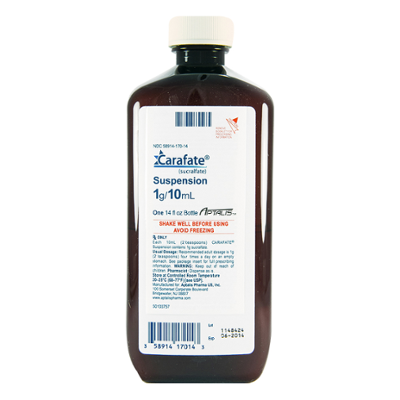
Many of these medications are also available as over-the-counter solutions for humans with acid reflux. While these may also be effective for dogs, always consult your vet before giving your dog any human medications to ensure the correct dose and frequency.
Dietary changes
Besides medication, diet modification is an essential component of acid reflux therapy. Vets often recommend a low-fat prescription diet to help reduce the production of stomach acid. This can also help with dogs and burping.
Your vet may also suggest changing the quantity and frequency of feedings. Feeding your dog smaller meals more often can help prevent the regurgitation that often happens when dogs eat large meals too quickly.
Probiotics and nutritional supplements
Probiotics are live microorganisms that help fight the harmful bacteria that cause inflammation and disease. Your vet may recommend adding a probiotic supplement to your dog’s daily regimen to help restore and balance your dog’s microbiome (the healthy gut bacteria that aid digestion.)
Many nutritional supplements and remedies claim to help reduce the impact of acid reflux in dogs. For example, slippery elm, licorice root, and ginger may help soothe the stomach lining. Ripe bananas may act as a natural antacid for dogs. And digestive enzymes can help support the pancreas in making digestion easier and more efficient.
If you are interested in how to treat acid reflux in dogs naturally, be sure to discuss options with your vet. It’s important to ensure they are safe for your dog and do not interfere with the treatment plan.
Surgery
If an endoscopy reveals the presence of a hiatal hernia, your veterinarian will discuss surgical correction of this congenital defect.
Whatever combination of treatment options your vet recommends, it’s important to start treating acid reflux in dogs right away. Effective treatment can help your dog avoid long-term complications like esophagitis, esophageal strictures, and even tumors of the esophagus from chronic inflammation.
How to Prevent Acid Reflux in Dogs

Prevention is always the best medicine, and nutrition can play a big role in helping prevent acid reflux in dogs. Feeding your dog a low-fat, low-protein diet, and avoiding high-fat treats is key. And even if your dog does develop acid reflux, you can prevent it from worsening by taking a proactive approach. Small, frequent meals and a balanced diet tailored to your dog’s needs can reduce acid reflux episodes and promote better digestion.
Related Conditions
- Esophagitis
- Regurgitation
- Hiatal Hernia
- Esophageal stricture
- Peptic ulcer
Dog Swollen Belly: 9 Causes
- 2024-10-25T02:25:47
- Sylvalyn Hammond, DVM
As a pet parent, discovering that your dog’s belly is swollen can be alarming. You might be left wondering if it’s something minor or if it requires immediate veterinary attention. A dog’s swollen belly can signal a wide range of conditions, from relatively harmless causes like overeating to life-threatening emergencies like bloat. Understanding what causes a dog’s stomach to swell and recognizing the associated signs can help you make informed decisions about your dog’s health.
In this article, we’ll explore the potential causes of a swollen belly in dogs, other signs to watch for, and when it’s necessary to seek veterinary care. We’ll also cover how a veterinarian diagnoses the problem and what treatment options are available to help your furry friend recover.
What Does a Swollen Belly in Dogs Look and Feel Like?

A swollen belly in dogs may present in different ways, depending on the underlying cause. The swelling can affect just one side of the abdomen or the entire belly. In some cases, the belly may feel soft and distended, while in others, it can feel firm or tight.
When we refer to a “swollen belly,” it’s important to understand that it can also be called abdominal distension or abdominal enlargement in dogs. These terms describe the outward appearance of a bloated or expanded abdomen. The swelling may be uniform or more pronounced in specific areas, and your dog might show signs of discomfort or pain when their belly is touched.
It’s not always easy to distinguish between a simple swollen belly and a more serious condition. A swollen belly due to overeating may feel soft and may not cause significant discomfort, whereas a distended abdomen due to something like bloat can be hard, tight, and painful.
Dog Swollen Belly: 9 Potential Causes

A swollen belly in dogs can be caused by a variety of conditions, ranging from mild to severe. Understanding the potential causes can help you recognize when veterinary attention is necessary. Here are some common causes of a swollen belly in dogs:
1. Intestinal Worms
Intestinal worms, such as roundworms, are a common cause of abdominal swelling, especially in puppies. These parasites can grow and accumulate in the intestines, causing significant bloating. Dogs with intestinal worms may also exhibit other symptoms like diarrhea, vomiting, a pot-bellied appearance, a poor hair coat, and weight loss. Treatment usually involves deworming medication, but severe infestations require urgent care to prevent complications, like life-threatening anemia or intestinal obstruction.
2. Bloat (Gastric Dilation)
Bloat, or gastric dilatation, occurs when a dog’s stomach fills with gas, fluid, or food, causing it to expand. In cases of simple bloat, the stomach does not twist, and mild cases of bloat are not life-threatening. However, bloat can still cause significant discomfort, and if serious bloat is left untreated, it can lead to issues like pressure on the lungs and restricted breathing. Bloat often presents with a distended, uncomfortable abdomen, restlessness, and repeated attempts to vomit. Prompt veterinary care is necessary to prevent complications.
3. Gastric Dilation-Volvulus (GDV)
Gastric dilatation-volvulus (GDV), commonly referred to as torsion, is a life-threatening emergency where the stomach not only fills with gas (bloat) but also twists on itself. This twisting cuts off the blood supply to the stomach and other organs, leading to rapid deterioration. Dogs with GDV typically have a hard, swollen abdomen and show signs of extreme distress, including retching without vomiting, drooling, and restlessness. Large, deep-chested breeds are more prone to GDV, and immediate emergency surgery is required to untwist the stomach and save the dog’s life.
4. Ascites (Fluid Accumulation)

Ascites refers to the accumulation of fluid in the abdominal cavity, which can cause a swollen or distended abdomen. This fluid buildup can be caused by several underlying conditions, including heart disease, liver disease, cancer, or severe infections. Dogs with ascites may also experience difficulty breathing if the fluid exerts pressure on the diaphragm. Veterinary evaluation is needed to determine the cause of the fluid buildup and to treat the underlying condition.
5. Peritonitis
Peritonitis is the inflammation of the lining of the abdominal cavity, typically due to infection, injury, or rupture of an internal organ (e.g., the intestines or bladder). This condition can cause severe abdominal swelling and pain. Peritonitis is a medical emergency and is often accompanied by other symptoms like fever, vomiting, lethargy, and loss of appetite. Immediate veterinary care is crucial to treat the infection and prevent further complications.
6. Tumors
Abdominal tumors, both benign and malignant, can cause a dog’s belly to swell. Tumors in the liver, spleen, or other abdominal organs can lead to either direct enlargement or cause secondary issues, such as ascites (fluid buildup). Dogs with abdominal tumors may exhibit other signs, such as weight loss, decreased appetite, or lethargy. Diagnostic imaging and possibly a biopsy are necessary to determine the nature of the tumor and the appropriate treatment.
7. Cushing’s Disease
Cushing’s disease occurs when a dog’s body produces too much cortisol, a hormone that regulates many functions. One of the hallmark signs of Cushing’s disease is a pot-bellied appearance due to fat redistribution and muscle weakness. Other signs include excessive drinking and urination, hair loss, and skin thinning. Treatment typically involves medication to regulate cortisol production, and long-term management is needed to control the symptoms.
8. Pregnancy

Pregnancy is a natural cause of abdominal enlargement in female dogs. As the puppies grow, the belly will become noticeably swollen, particularly in the later stages of gestation. In addition to a swollen abdomen, pregnant dogs may show signs of nesting behavior, reduced appetite, and increased fatigue. Parents of pregnant females will also notice changes in their nipples and swelling of their mammary glands. Veterinary care is highly recommended to monitor the health of the mother and her puppies throughout the pregnancy.
9. Obesity
Obesity is a common but non-emergent cause of abdominal enlargement. Overweight dogs may develop a pot-bellied appearance due to excess fat accumulation around the abdomen. While obesity doesn’t usually cause sudden swelling, it can put dogs at risk for many health issues, including joint problems, heart disease, and diabetes. A healthy diet and regular exercise are key to managing and preventing obesity in dogs.
Dog Swollen Belly: Other Signs to Watch For

A swollen belly is often accompanied by other symptoms that can give clues as to what might be going on. Here are some additional signs to watch for:
Drinking lots of water: Increased thirst, especially when combined with a swollen belly, could indicate Cushing’s disease, diabetes, or kidney issues.
Heavy breathing: Dogs with a distended abdomen may have difficulty breathing due to pressure on the diaphragm. This is especially concerning in cases of bloat or fluid accumulation in the abdomen (ascites) and requires immediate veterinary attention.
Not eating: Loss of appetite can be a sign of many underlying conditions, including tumors, infections, or digestive issues. A dog who refuses food along with a swollen belly should be evaluated by a veterinarian.
Vomiting: Vomiting is often associated with gastrointestinal issues like bloat, intestinal blockages, or parasites. Repeated vomiting with a swollen abdomen is a red flag for a medical emergency.
Lethargy: A dog who is unusually tired, weak, or uninterested in their normal activities may be suffering from a serious underlying issue. When combined with a swollen belly, lethargy could point to infections, cancer, or hormonal imbalances.
Pain or discomfort: If your dog shows signs of discomfort when you touch their belly, such as whining, growling, or flinching, it’s important to seek veterinary care. Painful swelling is often associated with conditions like bloat, tumors, or infections.
Restlessness: Dogs who are uncomfortable will typically pace endlessly or repeatedly get up and down. This can be a sign that your dog needs urgent medical care.
If you notice any of these symptoms together with a swollen belly, it’s a good idea to have your canine companion evaluated by a veterinarian as soon as possible.
How to Help a Dog with a Swollen Belly: Next Steps

The severity of a swollen belly in dogs can vary widely depending on the cause, but it’s always best to err on the side of caution and seek veterinary advice. While there may be a few situations where it’s okay to monitor the swelling at home, such as after mild overeating, most cases of abdominal distension should be evaluated by a veterinarian.
When you bring your dog to the vet for a swollen belly, they will perform a thorough physical exam and may recommend several tests to determine the cause of your dog’s swollen belly. These tests may include:
- Blood work: To check for infections, organ function, and hormone imbalances
- Urinalysis: To detect any issues with the kidneys or urinary system
- Radiographs (x-rays) or ultrasound: Imaging can help visualize what’s going on inside the abdomen, such as the presence of tumors, fluid accumulation, or abnormal organ structures
- Fecal tests: To check for intestinal parasites like worms
The treatment for a dog with a swollen belly will depend on the underlying cause. For example:
- Parasites: Medications will be prescribed to eliminate the worms
- Bloat: Immediate surgery may be required to untwist the stomach and prevent further complications
- Tumors: Treatment may involve surgery to remove the mass, followed by further therapies if necessary
- Cushing’s disease: This condition is typically managed with medication to control cortisol levels
- Obesity: A veterinarian will likely recommend a diet and exercise plan to help your dog lose weight
In some cases, lifestyle or dietary changes will be necessary to prevent recurrence of the condition. For example, if your dog has bloat, your veterinarian may suggest feeding smaller meals throughout the day and avoiding vigorous activity after eating.
How long it takes for your dog’s swollen belly to improve will depend on the cause and the treatment. For example, dogs with mild bloating from overeating may feel better within a few hours, while recovery from surgery for bloat or tumor removal may take weeks. In most cases, with prompt veterinary care, dogs can return to their normal selves after treatment, but ongoing monitoring may be necessary to prevent recurrence or manage chronic conditions.
Conclusion
A swollen belly in dogs is something that should never be ignored, as it can indicate a wide range of health issues, many of which are life-threatening. By being aware of the potential causes and accompanying signs, you can take prompt action to ensure your dog receives the appropriate care. If you’re ever in doubt, contacting your veterinarian for guidance is the best step you can take to help your beloved pet feel better and stay healthy.