Category: Pet Vaccinations
Great Pet Care - Pet health information — simplified.
Rabies Vaccine for Cats
- 2024-12-13T13:35:27
- Catherine Barnette, DVM
Rabies is a deadly viral infection that spreads in the saliva of infected animals. When a rabid animal bites another animal (or a person), rabies virus particles in the saliva enter the bitten animal via the bite wound. Over a period of weeks to months, the virus travels through the body, eventually reaching the brain and causing rabies in the bitten animal. Rabies is almost always deadly in people and pets, and it has been a recognized disease since ancient times.
Fortunately, thanks to widespread vaccination, rabies is now relatively uncommon in U.S. cats. In 2021, a total of 216 cats were diagnosed with rabies within the United States. In contrast, thousands of wild animals are diagnosed with confirmed rabies infection in the U.S. every year, and that number is surely an underestimate because most wild animals are never tested for rabies.
What Is the Rabies Vaccine for Cats?
Rabies vaccines are designed to prevent rabies infection. In most parts of the United States, rabies vaccination is required by law for both cats and dogs. This is because rabies is a zoonotic disease, meaning that it can affect both animals and people. Vaccinating dogs and cats helps to prevent rabies in people.
The first rabies vaccine was developed in 1885 by Louis Pasteur. This vaccine was designed for dogs, and the first vaccination campaigns for dogs began in the early 1900s. Over time, rabies vaccination expanded to cats. Since their development, rabies vaccines have been continually modified to make them safer and more effective.
Today’s rabies vaccines are considered very safe and very effective. Rabies vaccination is considered a core vaccine for cats, meaning that all cats should receive this vaccine early in life and continue to receive boosters over the course of their lifetime. All veterinarians administer rabies vaccines in their practice, so rabies vaccines are widely available to pet parents.
How Does the Rabies Vaccine for Cats Work?

Rabies vaccines for cats belong to a vaccine category known as “inactive” vaccines. The vaccine contains small amounts of killed (inactivated virus). When your cat’s immune system sees these viral fragments after receiving the vaccine, the immune system recognizes the fragments as foreign. This leads the immune system to develop an immune response against rabies virus, training the immune system to fight rabies exposure quickly.
A cat who has been vaccinated for rabies has an immune system that is trained to quickly recognize and attack the virus. If your cat is exposed to rabies, through the bite of a wild animal, the rabies vaccine will help your cat attack and destroy the virus before it causes an active infection.
Rabies Vaccination Schedule for Cats
A kitten’s first rabies vaccine should be given at 12-16 weeks of age. If you adopt your cat as an adult, the first rabies vaccine should be given as soon as possible.
Your cat will receive their first rabies vaccine booster one year after their initial vaccine. After this initial booster, further vaccine boosters will be given every 1-3 years, depending on the vaccine manufacturer’s instructions and your local legal requirements. Your veterinarian will determine whether your cat should receive a 1-year vs. 3-year rabies vaccine for cats.
| First rabies shot | First booster shot | Additional boosters |
| 12-16 weeks of age | 1 year after initial vaccine | Every 1-3 years (varies based on manufacturer and state/local laws) |
Possible Side Effects

Rabies vaccine reactions in cats are typically mild. Some cats experience mild discomfort at their vaccine site, and others may develop a slight fever or lethargy. These cats may have reactions like those seen in people receiving an annual flu vaccine.
In a study of 500,000 cats receiving vaccines, approximately 0.5 percent of vaccinated cats experienced a vaccine reaction that their owners reported to the veterinary hospital. Other cats may also have experienced a reaction, but it was mild enough that the owners did not contact their veterinarian.
The most common rabies vaccine reactions in cats include:
- Decreased appetite
- Lethargy
- Fever
- Soreness at vaccination site
- Mild swelling at vaccination site
Anaphylactic (allergic) reactions may also occur after vaccination. These reactions may be severe and life-threatening. Signs of anaphylaxis in cats include:
- Facial swelling
- Hives
- Itchiness
- Drooling
- Vomiting
- Difficulty breathing
- Pale gums
- Cold limbs
- Incoordination
- Seizures
- Coma
Anaphylactic reactions typically occur within minutes to hours of vaccination, and they require emergency treatment. Fortunately, anaphylactic reactions are very rare; they are reported to occur in 1-5 of every 10,000 cats receiving vaccines.
Finally, there is another form of uncommon reaction that can occur with vaccines in cats. Feline injection site sarcomas are a type of tumor that can occur after any injection, including vaccines. It is estimated that 0.3-1 in every 10,000 vaccines results in an injection site sarcoma. These tumors typically form months to years after receiving a vaccine.
Signs of injection sarcoma may include:
- A firm lump under the skin at an injection site
- Swelling, redness, or irritation around the lump
- A lump that is painful when touched
If you are concerned that your cat may have an injection site sarcoma, see your veterinarian.
Manufacturers of the Rabies Vaccine for Cats

There are several rabies vaccines available for use in cats. These vaccines are all effective against rabies virus, though there are slight differences between vaccines.
Nobivac (Merck Animal Health), Vanguard (Zoetis), Rabvac (Elanco), and Imrab (Boehringer Ingelheim) are conventional rabies vaccines for use in cats. These vaccines are all commonly used by veterinary practices, and they are all available in both 1- and 3-year formulations.
PureVax (Boehringer Ingelheim) differs from the other vaccines, because it is the only feline rabies vaccine that is made without adjuvants. Adjuvants are substances that boost the immune reaction triggered by a vaccine, but they are also thought to play a role in vaccine side effects. In addition to potentially reducing the risk of vaccine reactions, PureVax is also delivered in a smaller injection volume than other, conventional rabies vaccines. While this vaccine offers potential benefits, it is more expensive than other rabies vaccines. Like other rabies vaccines, PureVax is available in both 1- and 3-year formulations.
Your veterinarian will determine the best rabies vaccine for your cat. Most veterinarians only stock one formulation of rabies vaccine, and that is the formulation that they feel offers the most benefits for their patients and clients.
| Manufacturer | Product Name | Product Name |
| Boehringer Ingelheim | Imrab (1- and 3-year) Imrab TF (1- and 3-year thimerosal-free) | PureVax (1- and 3-year) |
| Elanco | Rabvac (1- and 3-year) | |
| Merck Animal Health | Nobivac (1- and 3-year) | |
| Zoetis | Vanguard (1- and 3-year) |
Cost of the Rabies Vaccine for Cats
Cat rabies vaccine costs may vary, depending on numerous factors. In general, PureVax is more expensive than other vaccines. Having your cat vaccinated for rabies will likely also include a veterinarian exam, as well as paying for local pet licensing.
The cost of a thorough veterinary exam, rabies vaccine, and local license (if required) will be approximately $100-$200.
Does Your Cat Need to Be Vaccinated for Rabies?

All cats should be vaccinated for rabies, because all cats are at risk of this deadly infection. Even indoor cats need rabies vaccines; there have been countless reports of indoor cats that escape their home and/or bats and other wildlife entering a home. Rabies isn’t just an inconvenience — infection is fatal for cats.
Rabies vaccination also protects you, the pet parent. As a veterinarian, I have seen cats who were infected with rabies. In many cases, these cats exposed numerous family members, requiring everyone in the family to receive post-exposure rabies prophylaxis. Fortunately, post-exposure prophylaxis is effective when given quickly. Unfortunately, this treatment is uncomfortable and expensive. And, if your cat develops rabies but dies before being diagnosed, there is a possibility that you could become infected without knowing it. Rabies infection is almost always fatal without post-exposure treatment.
Finally, rabies vaccination has legal implications. If your cat is bitten by a wild animal, law enforcement may require 4-6 months of quarantine or even euthanasia. If your unvaccinated cat bites someone, law enforcement may also require quarantine (for up to 10 days). In many cases, quarantine must take place outside of your home; this is not only stressful for your cat, but it can also become very expensive for you. (I have seen clients spend thousands of dollars to quarantine their cat at a veterinary hospital after the cat received a bite wound while roaming outdoors!) Keeping your cat up-to-date on rabies vaccines reduces the likelihood of expensive fines, quarantines, and other stressful scenarios that can ensue when you do not follow legal requirements.
If you have concerns about rabies vaccination, talk to your veterinarian. Work together to create a plan to protect your cat against rabies as safely as possible.
References
- Ma, Xiaoyue et al. “Rabies surveillance in the United States during 2021.” Journal of the American Veterinary Medical Association vol. 261,7 1045-1053. 8 Mar. 2023, doi:10.2460/javma.23.02.0081
- American Animal Hospital Association. “Adverse Postvaccination Reactions.” Aug. 2020. Retrieved from https://www.aaha.org/resources/2020-aahaaafp-feline-vaccination-guidelines/adverse-postvaccination-reactions/
Vaccine Reactions in Dogs: Signs and What to Do
- 2024-01-16T22:08:14
- Sylvalyn Hammond, DVM
Vaccinations save lives and are an important part of keeping dogs safe and healthy. By vaccinating early and regularly, serious and even fatal infectious diseases, like canine parvovirus and rabies, can be avoided entirely. While the benefits of vaccinations greatly outweigh the risks, vaccine reactions in dogs are possible and do happen. Here’s everything dog owners need to know about dog vaccine reactions.
Do Dogs Develop Vaccine Reactions?
Modern vaccines are extremely safe and effective, but dogs can still experience vaccine reactions. In almost all cases, dog vaccine reactions are mild and do not require treatment, but in very rare cases, more severe reactions can occur and require immediate medical intervention.
In 2021, a study published by the National Institute of Health evaluated 1,226,159 dogs receiving 3,439,576 vaccine doses. Out of all these dogs and vaccines, only 4,678 vaccine reactions were recorded. This equates to 38.2 reactions per 10,000 dogs, or in other words, only 0.382 percent. [1] Additionally, the majority of these dog vaccine reactions were mild and self-limiting, such as soreness and lethargy.
Small breed dogs have a higher risk for vaccine reactions. As a dog’s size increases, the risk of an adverse vaccine reaction decreases. Studies have also shown that neutered dogs have a slightly higher chance of having an adverse vaccine event [2]. Lastly, the more vaccines that are administered at one time, the higher the risk of an allergic reaction.
Dogs with immune-mediated diseases are not at a higher risk for vaccination reactions despite a popular theory that vaccination could induce a relapse of that disease. Fortunately, research does not support a link between vaccination and the development of immune-mediated diseases.
Most Common Vaccines That Cause Reactions
The highest rate of vaccination reactions in dogs occurs after the Lyme disease vaccination. [1] This may be due to the size of Borrelia burgdorferi, the bacteria that causes Lyme disease, or one of the ingredients used to help induce an appropriate immune response. Reactions after the Lyme vaccine are most often limited to local pain at the injection site and resolve without intervention.
Historically, the leptospirosis vaccination triggered a higher rate of dog vaccination reactions. This was due to both the size of the bacteria and the bovine serum used to increase the efficacy of the vaccinations. In response to the higher rate of reactions to the vaccine, the original formulation was withdrawn and revised. Today’s leptospirosis vaccine utilizes only a portion of the main bacteria, and in a recent study of over 1 million dogs, the leptospirosis vaccine was not found to be more likely to cause a reaction when compared to other vaccines. [3]
Types of Vaccine Reactions in Dogs

Most vaccine reactions in dogs are systemic, meaning that the whole body is affected. This could be general malaise after a vaccination, a mild allergic reaction, or a more severe allergic reaction known as anaphylaxis. Systemic vaccination reactions in dogs can also be delayed, in which case the reaction happens 24-48 hours after the vaccine was administered. Delayed vaccine reactions are exceedingly rare.
Localized vaccine reactions are also possible. These types of reactions only affect the animal where the vaccine was given. Usually, the local reaction is soreness or mild swelling, both of which resolve in a few days. Some dogs, however, will form small, firm bumps under the skin where the vaccine was given. For these, veterinarians use the 3-2-1 rule. The bump is not a concern unless it persists for three months after an injection, becomes larger than 2 centimeters in diameter, or continues to increase in size one month after an injection.
Signs of Dog Vaccine Reactions
After a vaccine is injected, it will stimulate an inflammatory response. This ensures that the body recognizes the antigen, triggers the immune system, and creates the antibodies needed for protection. Therefore, mild inflammatory symptoms after vaccinations are expected and common. Dogs with mild, common vaccination reactions can display one or more of the following:
- Soreness or swelling at the injection site
- Lethargy
- Mild fever
- Reduced energy
- Decreased appetite
- Sneezing after a nasal vaccine
These symptoms are all considered part of the normal vaccination process and are a sign that the body is working toward creating the protective response. Pet parents should take note of these and keep a close eye on their dog for resolution of the symptoms, but treatment is not usually necessary, and no modifications need to be made for future vaccinations.
Signs of serious vaccine reactions in dogs are as follows:
- Vomiting or diarrhea
- Puffy eyes
- Swollen muzzle
- Small, raised bumps on the body
- Difficulty breathing
- Collapse
These symptoms can indicate anaphylaxis, a severe and exaggerated immune response to the vaccine. Anaphylaxis can be life-threatening without treatment. If a dog displays any of these symptoms, you should seek veterinary care right away. Typically, anaphylaxis occurs within the first hour after the vaccine was given, but it can occur up to 24 hours later.
Treating Vaccine Reactions in Dogs
If a dog is having a serious vaccine reaction, immediate treatment is necessary. Fortunately, veterinarians can effectively treat vaccine reactions in dogs. The sooner a veterinarian is able to intervene, the easier it will be to stop the inflammatory cascade driving the allergic reaction.
In most cases, dog vaccine reactions are treated with a combination of injectable antihistamines and steroids. Signs usually resolve shortly after a veterinarian administers these medications.
More severe vaccine reactions in dogs may require hospitalization for intravenous medications, fluid therapy, and monitoring.
Vaccine Reactions in Dogs: Things to Keep in Mind

Recently, exaggerations of potential adverse effects have discouraged dog owners from having their canine companions vaccinated. This is mostly due to the development of the internet and social media, which allow people to spread their opinions and re-share data out of context. Much of the hesitancy regarding vaccines is the result of the negative effects and lower efficacy of the earliest vaccines, in spite of the fact that these issues have been resolved.
Vaccinations have saved more lives than any other medical intervention, and while dog owners should be aware of possible vaccine reactions, they should take comfort in knowing that canine vaccinations are safe and effective, dog vaccine reactions are very rare, and veterinarians are well equipped to treat serious adverse events if they do occur.
References
- Tizard IR. “Adverse consequences of vaccination.” Vaccines for Veterinarians. 2021:115–130.e1. doi: 10.1016/B978-0-323-68299-2.00019-8. Epub 2020 Jul 10. PMCID: PMC7348619. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7348619/#:~:text=Out%20of%201%2C226%2C159%20dogs%20receiving,%25%20were%20considered%20%E2%80%9Cvaccine%20reactions%E2%80%9D
- Moore GE, Guptill LF, Ward MP, Glickman NW, Faunt KK, Lewis HB, Glickman LT. “Adverse events diagnosed within three days of vaccine administration in dogs.” J Am Vet Med Assoc. 2005 Oct 1;227(7):1102-8. doi: 10.2460/javma.2005.227.1102. PMID: 16220670. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/16220670/
- Brooks, Wendy. “Vaccine allergic reactions in dogs and cats.” Veterinary Information Network. Retrieved from: https://www.vin.com/vetzinsight/default.aspx?pid=756&catId=102903&id=4951409&ind=808&objTypeID=1007
Canine Influenza Vaccine: All About the Dog Flu Shot
- 2023-06-19T15:59:21
- JoAnna Pendergrass, DVM
Canine influenza, or dog flu, is a highly contagious respiratory disease. Caused by the canine influenza virus, canine influenza was first reported in dogs in the United States in 2004 and has since been reported in 46 states. Most of these reports have been isolated disease outbreaks, indicating that canine influenza hasn’t gained a strong foothold in the general dog population.
Many dogs have not been exposed to the canine influenza virus, meaning they don’t yet have immunity to the disease. According to the American Veterinary Medical Association, about 80 percent of dogs exposed to the virus will get sick with symptoms like a soft, moist cough, nasal discharge, and lethargy.
Canine influenza is rarely fatal, but it can make dogs feel crummy. Because this disease is highly contagious, protecting dogs from exposure to the canine influenza virus is important.
The canine influenza vaccine is the best way to protect dogs from this disease. The more dogs that get vaccinated, the less the virus will be able to circulate throughout the dog population and cause disease.
What Is the Canine Influenza Vaccine?
There are currently two canine influenza vaccines, and both are FDA approved. They are available in veterinary practices nationwide, with no need to see a veterinary specialist to get the vaccine.
This vaccine is considered a non-core vaccine, meaning that not every dog needs to receive it. The 2022 American Animal Hospital Association (AAHA) Guidelines state that non-core vaccines are “recommended for some dogs based on lifestyle, geographic location, and risk of exposure.”
Because the canine influenza vaccine is not a core vaccine, there are currently no legal requirements on the state or municipal level for dog flu vaccination. However, certain animal facilities, such as doggie daycares and boarding facilities, may require dog flu vaccination to prevent the spread of the disease in the facility.
How Does the Flu Shot for Dogs Work?
The canine influenza vaccine is a bivalent vaccine, meaning that it protects against the two strains of the canine influenza virus: H3N2 and H3N8.
The vaccine is made up of inactivated (killed) canine influenza virus. The killed virus will stimulate the immune system without causing disease. However, compared with other vaccine formulations, killed virus vaccines may have a shorter duration of immunity and may cause more negative side effects.
The canine influenza vaccine also contains adjuvants that help boost the immune response.
Note that the vaccine does not provide 100 percent protection against the dog flu. However, it does help reduce the duration and severity of illness in dogs that get the disease.
Canine Influenza Vaccination Schedule for Dogs

According to the AAHA Vaccination Guidelines, the canine influenza vaccination schedule is two doses 2 to 4 weeks apart, followed by an annual booster. It can be given to any dog who is over 8 weeks old.
Possible Side Effects of the Dog Flu Shot
As with all dog vaccines, the canine influenza vaccine comes with potential side effects. Most dogs tolerate the vaccine very well and have either mild or no side effects, while some dogs may have severe adverse reactions that require medical attention.
Here are the more common and mild side effects of the canine influenza vaccine:
- Pain and swelling at the injection site
- Lethargy
- Reduced appetite
Serious side effects are listed below:
- Hives
- Collapse
- Persistent vomiting or diarrhea
- Swelling of the face, neck, eyes, or muzzle
Seek immediate veterinary care if your dog develops severe side effects after vaccination.
The canine influenza vaccine does not react with medications or other vaccinations.
Manufacturers of the Canine Influenza Vaccine for Dogs
Merck and Zoetis each manufacture the canine influenza vaccine.
Merck’s canine influenza vaccine is the Nobivac Canine Flu Bivalent. It was the first vaccine to demonstrate effectiveness against both strains of the virus. It received FDA approval in 2017 and can be given to dogs 7 weeks and older.
The canine influenza vaccine from Zoetis is called Vanguard CIV H3N2/H3N8. It also received FDA approval in 2017 and can be given to dogs 8 weeks and older.
Zoetis does have monovalent canine influenza vaccines that protect against one or the other strain of canine influenza virus. However, on their website, the company “strongly recommends that these vaccines be used only if a dog is lacking vaccination against one of the two strains, and then continue with the use of Vanguard CIV H3N2/H3N8.”
Costs of the Canine Influenza Vaccine
The cost of the vaccine will vary according to veterinary practice and geographic location. Generally, the vaccine costs approximately $20 to $55.
If your veterinarian performs a physical exam before administering the vaccination, expect to also pay for the cost of the office visit. The vaccine and office visit together could cost upwards of $100.
Low-cost vaccine clinics provide an inexpensive option to get your dog vaccinated. Contact your local low-cost vaccine clinics to ask whether they have the canine influenza vaccine.
Does Your Dog Need the Flu Shot?

That depends. Here are some factors that increase a dog’s risk of getting the dog flu:
- Traveling extensively
- Going to doggie daycare
- Staying at a boarding facility
- Frequently visiting the dog park
- Participating in social events, such as dog shows and agility events
In older dogs, respiratory disease and heart disease can increase the risk of getting the dog flu. Also, brachycephalic (smoosh-faced) breeds are at higher risk of canine influenza because their facial structure makes it harder for them to breathe.
Talk with your veterinarian if you’re unsure whether the flu shot is right for your dog.
Everything You Need To Know About Cat Vaccinations
- 2021-03-30T16:09:05
- Emily Bergquist
Cat vaccinations are one of the most debated topics in the pet world. Knowing what vaccinations for your cat are necessary and which ones are optional can be confusing.
In this article, we provide detailed answers to some of the most frequently asked questions on cat vaccinations.
Do I Need to Vaccinate My Cat?
The answer to this question is yes.
According to the American Association of Feline Practitioners, your cat should be vaccinated. Cat vaccinations are also scientifically and medically proven to be beneficial. Such vaccinations minimize the transmission of fatal diseases and viruses that can cause lifelong illness in cats.
Furthermore, vaccinating your cat against diseases such as rabies ensures that you and other animals in your home are safe from fatal diseases.
When Should You Vaccinate Your Cat?
If you just brought a kitten into your home, you’ll first need to find out if they are vaccinated.
Kitten vaccines typically start between 6 to 8 weeks of age, depending on the vaccine, medical history, and the person administering the vaccine. The vaccines are then administered in a series every three to four weeks until the kitten reaches at least 16 weeks of age. This series of vaccines are not the same for every kitten, and will vary slightly depending on when they received their first vaccines and their lifestyle. These vaccines are typically boostered at 1 year of age.
If you have an adult cat who has never been vaccinated, you’ll need to talk to your vet. The vet will advise you on the best vaccines for your fur baby after considering their age, lifestyle, breed, location, and pre-existing medical conditions.
Adult cats who have already been vaccinated will need booster shots after 1-3 years, depending on the duration of the vaccine, location, and lifestyle.

What vaccines do I need to give my cat?
According to the Feline Vaccination Advisory Panel guidelines, cat vaccines are divided into two categories:
- Core shots
- Non-core shots
Core Cat Vaccines
Core vaccines are required for all cats. These vaccines protect against diseases that are highly contagious and fatal. The core vaccines also have minimal adverse effects on cats.
The two essential vaccines for cats are:
- Rabies
- FVRCP
- Feline viral rhinotracheitis
- Feline calicivirus
- Feline panleukopenia virus or feline distemper
Let’s take a closer look at each of these vaccines:
Rabies vaccine
The rabies virus is fatal to both humans and animals. Most states require that your cat be vaccinated against rabies. Cats get rabies after being infected by other sick animals, and they then pass on the virus to others. Some of the symptoms of this disease in your cat include wobbly while walking (ataxia), aggression, and death.
The FVRCP vaccine
This vaccine is also known as the distemper shot. It’s a single shot given to protect your cat against the three viruses below:
- Feline viral rhinotracheitis (FVR): This virus, also known as feline herpes, is caused by feline herpesvirus type 1 (FHV-1). It affects a cat’s respiratory system and is characterized by conjunctivitis, nasal congestion, and sneezing. The disease can also lead to pneumonia.
- Feline calicivirus (FCV): Feline calicivirus affects a cat’s upper respiratory organs. Signs of this virus include oral ulcerations, sneezing, nasal discharge, gingivitis, and even death.
- Feline panleukopenia virus (FPV): This highly infectious illness is characterized by poor appetite, lack of energy, diarrhea, vomiting, and even sudden death in kittens.
Your cat should get booster shots of these core vaccines one year after the initial shots. The FVRCP vaccine should be administered annually to outdoor cats. Cats who are low risk and live an indoor existence without any known exposure, like open screens, can wait to get the vaccine every three years.
Non-Core Cat Vaccines
Your fur baby may need extra vaccines depending on the prevalence of illness in your area and the amount of time they spend outdoors. These shots are non-core vaccines. Some of the most common ones include:
- Chlamydia: This shot protects your cat from chlamydia, a bacterial infection that leads to conjunctivitis. This shot is sometimes part of the FVRCP vaccine.
- Feline leukemia virus (FeLV): This vaccine is highly recommended for outdoor cats. The virus is transmitted through body fluids, such as saliva and urine. Although some cats recover from this disease, others suffer from secondary illnesses, such as anemia or lymphoma, once the disease goes past the latency stage.
- Bordetella: This vaccine is strictly for catteries and animal shelters in which Bordetella infection is a confirmed issue for their entire population. This disease is highly contagious and causes respiratory symptoms, such as sneezing, fever, difficult breathing, and nasal discharge.

Do Cat Vaccines Have Severe Side Effects?
Each of the vaccines highlighted above carries a given amount of risk. However, these risks are much lower than the risk of your cat getting the highlighted diseases.
The effects of these vaccines on your cat are often mild, and they occur in only about 0.5 percent of all vaccinated cats. Death and other adverse outcomes are extremely rare. If your cat has no history of vaccine reactions, they will likely be okay.
Some of the symptoms you can look out for that may be an indication of a vaccine reaction in cats include:
- Fever
- Lameness
- Swelling and redness on the injection area
- Vomiting
- Lethargy
- Hives
- Diarrhea
If you notice any of these signs, consult your vet immediately to ensure your cat gets immediate care.
Cats in particular are at risk for injection site sarcomas from receiving vaccines and other injections. Although rare, these malignant tumors will develop at the site of an injection. Fortunately vaccines have been developed to minimize the risk of these tumors. Speak with your veterinarian about the best option for your cat. If you feel a bump has developed at the site of an injection, see your doctor as soon as possible.
Keep Track of Your Cat’s Vaccination Records
After vaccinating your cat, stay organized by keeping track of your cat’s vaccination records. Consider setting vaccination reminders, so you’ll get a notification when your cat is due for another round of shots.
Understanding the importance of vaccinating your cat is vital to being a good pet parent. If you have a new kitten or your adult cat isn’t up-to-date with their vaccinations, schedule a visit with a vet immediately so you can agree on a vaccination schedule.
DHPP Vaccine for Dogs
- 2020-07-22T16:06:33
- Catherine Barnette, DVM
All dogs, from puppyhood through adulthood, should be vaccinated appropriately with the DHPP vaccine. The DHPP vaccine protects against a number of severe viral illnesses in dogs, including distemper, adenovirus, parainfluenza, and parvovirus. Some of these diseases were associated with significant outbreaks and mortality in dogs prior to the development of vaccines.
The DHPP vaccine for dogs is a core vaccination, which means that it is recommended for every dog, regardless of lifestyle.
What is the DHPP Vaccine?
The DHPP vaccine, which may also be referred to as the DAPP vaccine or DA2PP vaccine, protects dogs against four unique illnesses. These illnesses include:
Distemper virus: Canine distemper is a virus that affects the respiratory, gastrointestinal, and nervous system of dogs. It is typically spread via coughing and sneezing, although spread can also occur in a number of other ways. There is no cure for distemper virus and infection is often fatal. In dogs that survive, neurologic damage may be permanent.
Hepatitis/Adenovirus-2: Canine adenovirus 2 (CAV-2) is included in vaccines for two separate reasons. First, CAV-2 can cause kennel cough in dogs. Second, and more importantly, CAV-2 is closely related to CAV-1, a virus that causes a potentially-fatal liver infection in dogs. Vaccinating against CAV-2 protects dogs against CAV-1 and infectious canine hepatitis. (Some DHPP vaccines also provide direct immunity against CAV-1).
Parvovirus: Canine parvovirus is most common in puppies, but it can affect dogs of any age. Parvovirus attacks the gastrointestinal tract, causing vomiting and diarrhea that can be fatal, even with aggressive treatment. Additionally, parvovirus suppresses the immune system and makes infected dogs more susceptible to a number of other infectious diseases. Most infected dogs will die without treatment. With aggressive treatment, many (but not all) dogs survive infection.
Parainfluenza virus: Canine parainfluenza virus is a highly contagious virus that causes coughing and other respiratory signs.
The individual vaccine components included in the DHPP vaccine were each developed uniquely, but they have since been combined into a single injection for ease of administration.
The DHPP vaccine for dogs is carried by nearly every veterinary practice in the United States. It is regarded as a core vaccine, which means that it is recommended for all dogs, regardless of their risk or lifestyle. While the DHPP vaccine is strongly recommended for all dogs, it is not legally required.
How Does the DHPP Vaccine for Dogs Work?

The DHPP vaccine contains small amounts of modified distemper virus, CAV-2, parvovirus, and parainfluenza virus. These viruses have all been modified in such a way that they cannot trigger an actual infection, but they can still trigger an immune response.
When your dog is vaccinated against these viruses, your dog’s immune system learns to recognize these viruses. This primes the immune system to attack these viruses if they enter the body via a natural infection.
DHPP Vaccination Schedule for Dogs
Dogs should receive their first DHPP vaccines as puppies. This vaccine is typically started at the first puppy visit, as early as 6 weeks of age. It is then repeated every 3-4 weeks until the puppy is 16-20 weeks old (depending on breed and risk).
It’s important to ensure that your puppy receives the entire recommended vaccine series, because stopping the vaccine series too early could put your dog at risk of disease. If your puppy gets sick unexpectedly, and you have a health and pet care credit card, such as CareCredit, it can give you the peace of mind needed to care for your canine companion.*
Once the initial “puppy shots” are completed, your dog is protected against all four viruses for one full year. A DHPP booster should be administered one year after the last vaccine in the puppy series. After the one-year booster, a booster vaccination should be administered every three years.
| First DHPP shot | Additional DHPP shots | First DHPP booster shot | Additional DHPP booster shots |
| In puppies, as early as 6 weeks old | Every 3-4 weeks until puppies are 16-20 weeks old | One year after final DHPP puppy shot | Every 3 years following the first booster |
Side Effects of the DHPP Vaccine for Dogs

Vaccines trigger an immune response in dogs, which is how they provide immunity. Therefore, you may see clinical signs that your dog’s immune system is working. Mild lethargy and soreness at the site of the vaccine are relatively common side effects after vaccination, similar to how you might feel after a vaccine.
In rare cases, a more severe allergic vaccine reaction may occur. These reactions may be accompanied by hives, facial swelling, itching, vomiting, diarrhea, weakness, or collapse. If you see signs of an allergic reaction, contact your veterinarian immediately.
Common side effects of vaccines:
- Lethargy
- Pain at the injection site
Call your veterinarian if you observe any of the following:
- Hives
- Facial swelling
- Itching
- Vomiting
- Diarrhea
- Weakness
- Collapse
DHPP Vaccine Medication Reactions
While there are no medications that react directly with the DHPP vaccine, corticosteroids (such as prednisone) should be avoided at the time of vaccination, if possible. Steroids suppress the immune system’s response and may decrease the likelihood that your dog develops an appropriate immune response to vaccination.
Additionally, your veterinarian may recommend separating the DHPP vaccine from other vaccinations. While it is not technically unsafe to administer multiple vaccines at the same time, the administration of multiple vaccines in a single visit is associated with an increased risk of vaccine reactions, especially in small dogs.
Manufacturers of the DHPP Vaccine for Dogs
There are several different manufacturers that produce DHPP vaccines. Available vaccines include:
| DHPP Vaccine Manufacturer | Vaccine Name |
| Merck Animal Health | Nobivac Canine DAPPv |
| Zoetis | Vanguard Plus 5 |
| Elanco | Duramune Max 5; ULTRA Duramune |
The ULTRA Duramune vaccine from Elanco is unique in that it is only half the volume of other DHPP vaccines. This is intended to minimize discomfort and the risk of vaccine reactions. With the exception of this vaccine, the other three vaccines are very similar.
Cost of the DHPP Vaccine for Dogs

The cost of the DHPP varies, based upon your area’s cost of living and which vaccine your veterinarian is using. In general, you can expect to pay $20-$40 for the DHPP vaccine. The vaccine is typically administered in conjunction with a physical exam, which typically costs approximately $50-$80.
If you have pet health insurance, your plan may help cover some vaccine costs. Look for plans with preventative care or wellness package add-ons that cover expenses associated with keeping your pet healthy. The CareCredit credit card is another good solution to consider, because it can help you manage pet care costs, such as vaccinations. It can be used at any provider in the CareCredit network, and it allows you to pay over time with flexible financing options.*
Does Your Dog Need the DHPP Vaccine?
Distemper virus, CAV-2, parvovirus, and parainfluenza are severe health threats. Distemper virus and parvovirus, in particular, are highly contagious and can be fatal. The DHPP vaccine is regarded as a core vaccine. This means that all dogs should receive this vaccine, regardless of their lifestyle or individual risk.
Some dogs may have severe vaccine reactions to DHPP that are life threatening. In these cases, talk with your veterinarian about your options.
*Subject to credit approval. See carecredit.com for details.
This information is shared solely for your convenience. Neither Synchrony nor any of its affiliates, including CareCredit, make any representations or warranties regarding the products described, and no endorsement is implied. You are urged to consult with your individual veterinarian with respect to any professional advice presented.
Feline Leukemia Vaccine (FeLV) for Cats
- 2020-06-26T17:26:36
- Emily Swiniarski, DVM
Feline leukemia virus (FeLV) is found in approximately 2 percent of cats in the United States. The disease is found worldwide in varying amounts. FeLV suppresses, or decreases, the immune system making cats more susceptible to a variety of infections and cancer.
Studies show that cats infected with FeLV live shorter lifespans than cats without it. Because of the effects of this disease, it is important to protect your cat from infection. Vaccination can help with that, but it isn’t necessary for all cats.
Read below to understand if your cat needs the FeLV vaccine.
What is the FeLV Vaccine?
The FeLV vaccination protects cats against the symptoms of feline leukemia virus. It was first created and placed on the market in 1985. This vaccine has been approved by the United States Department of Agriculture (USDA). Pet parents can go to any veterinary clinic in the country and request the FeLV vaccine. This vaccination is not known to be required by any level of law in the US.
How Does the FeLV Vaccine Work?

After vaccination, a cat’s immune system creates a memory for a specific virus—both by producing cells that fight the disease and by producing immunoglobulins, important proteins that find the virus, stick to it, and signal the body to destroy it.
If a cat is not vaccinated against a particular virus, his immune system will require days to weeks to mount an effective immune response when he is exposed to it. If, however, a cat IS vaccinated against a particular virus, his immune system will kick in within minutes to hours after exposure!
Some studies have shown that the FeLV vaccine may prevent symptoms (signs) of FeLV disease, but not necessarily infection. Testing of cats exposed to FeLV after vaccination shows the presence of proviral DNA of FeLV in the body. This is not an active infection, and the virus should not replicate or infect the cat. However, it is possible that in future years FeLV could begin to replicate (or grow) and cause FeLV disease.
There are currently 2 different kinds of FeLV vaccination:
Inactivated virus vaccine: this means the actual virus in its complete form is altered in the laboratory so it can no longer infect cats—also known as “killed” vaccines.
Recombinant canarypox vector vaccine: This means an important piece of FeLV was placed into another harmless virus called canarypox. This live canarypox virus will express important proteins from FeLV that will then stimulate an immune response, but FeLV itself is not present in its entirety
Feline Leukemia Vaccination Schedule for Cats
Before any cat is vaccinated against FeLV, they need to be tested for FeLV. There are a variety of tests, and your veterinarian will choose the exact test based on what his/her clinic uses. If your cat tests positive for an infection, it is not recommended to vaccinate against FeLV.
Every cat receiving the FeLV vaccine for the first time receives two doses, 2-4 weeks apart. The duration of immunity—or the length of time that the vaccine protects your cat—is proven at 1 year in most vaccines. Studies have shown that several vaccines can provide 2 years of protection, but not all cats will experience full protection at 2 years. Your veterinarian will help you decide your cat’s level of risk and whether you can wait 2 years until the next vaccination.
| First FeLV Shot | FeLV Booster | Additional FeLV Shots |
| Any age, following virus testing | 2-4 weeks after initial vaccine | Every 1-2 years |
Side Effects of the Feline Leukemia Vaccine

As with any cat vaccination, the FeLV vaccination can cause the following side effects:
- Local swelling and/or pain (vaccine should be given in the left rear leg)
- Decreased activity
- Fever of short duration
- Granuloma (non-cancerous growth from chronic inflammation)
In rare cases, cats can develop injection site sarcomas, a severe form of skin cancer that is very invasive and cannot be easily treated. Approximately 1 in 10,000 cats who are vaccinated will develop this disease. Other types of injections can cause this rare disease as well, such as long-acting steroids.
Speak to your veterinarian if you are concerned with this rare side effect. Ask your veterinarian where they inject vaccines in cats. An outdated veterinary practice was to give vaccines to cats in between the shoulder blades, and this is associated with a much higher risk of developing sarcoma. Vaccines should be given low on your cat’s hind leg (usually the left) or on the tail. This way, if an injection site tumor grows, the limb can easily be amputated to remove the tumor and all affected tissue.
Manufacturers of the FeLV Vaccine for Cats
There are four licensed manufacturers of the FeLV vaccine in the U.S. They all create FeLV vaccines alone, as well as some create a combined product with other viruses. Either killed or canarypox vector vaccines are made.
The following manufacturers make FeLV vaccinations:
| Manufacturer | Type of Vaccine(s) | Product Name | Product Name |
| Boehringer Ingelheim | Killed vaccine, Canarypox vector vaccine | PUREVAX | |
| Elanco | Killed vaccine | ULTRA Fel-O-Vax | |
| Merck Animal Health | Killed vaccine | Nobivac Feline 2-FeLV | NOBIVAC Feline 1-HCPCH+FELV |
| Zoetis | Killed vaccine | FELLOCELL FeLV | LEUKOCELL 2 |
Cost of the FeLV Vaccine for Cats
Individual FeLV vaccines will cost approximately $25-$50 each at a veterinary clinic. This does not include the examination fee at each appointment. Your cat will need to be tested for FeLV before receiving his first vaccine, which also generally ranges anywhere from $25-$100, depending on the type of test.
Does Your Cat Need the Feline Leukemia Vaccine?

Kittens are recommended by feline specialty groups to be routinely vaccinated against FeLV since they are most susceptible to contracting FeLV. Not every kitten will have exposure, however, so not every veterinarian will recommend vaccination of your kitten.
After the first round of FeLV vaccination (2 boosters), whether or not your cat should be vaccinated 1 year later depends on if there is any potential for exposure to FeLV. Adult cats build natural immunity to the FeLV disease, so vaccinating adult cats should only occur if there is substantial risk of exposure to FeLV.
Possibilities for FeLV exposure include:
- If your cat goes outdoors.
- If your cat spends considerable time on porches or at screened windows and comes into close contact with roaming cats.
- If you decide to adopt or purchase a new cat that is either FeLV infected or has not been tested.
- If you foster (temporarily care for) any cat whose status of FeLV infection is unknown.
- If your cat goes to cat shows.
- If you routinely board your cat.
Your veterinarian can help you determine whether your cat should be vaccinated against FeLV.
Rattlesnake Vaccine for Dogs
- 2020-06-24T16:42:18
- Sarah J. Wooten, DVM
People who love to spend time outdoors with their dogs understandably are concerned about snake bites. Venomous snakes are found in 46 U.S. states, and it is estimated that over 150,000 animals—mostly dogs and cats—are bitten by poisonous snakes in the U.S. every year.
The majority of bites come from pit vipers, including rattlesnakes. The severity of snake bites range depending on the level of toxicity and amount of snake venom in the bite, the location of the bite (bites to faces or vital organs are more severe), how many times a dog was bitten, and the size of the dog, with smaller dogs being at higher risk.
Dogs bitten by a rattlesnake can develop severe swelling around the bite. Snake bites can also cause severe pain, weakness, low blood pressure, and blood-clotting abnormalities. Dogs that have been bitten by a rattlesnake require immediate, emergency care that is often expensive and requires hospitalization. To treat rattlesnake bites, veterinarians usually administer an antivenin, an antiserum that contains antibodies that neutralize the poisonous effects of rattlesnake venom.
Dog parents looking to protect their pooch against snake bites may have heard about a rattlesnake vaccine for dogs. But does this vaccine actually work and does your dog need it?
What is the Rattlesnake Vaccine?
The rattlesnake vaccine for dogs has been available since 2003. It contains inactivated venom from the western diamondback rattlesnake, adjuvant (an agent that improves the immune response of a vaccine), and preservatives.
Like all dog vaccines, the rattlesnake vaccine is monitored by the USDA. It is offered through local veterinarians, mostly in areas that are endemic for rattlesnakes, such as the western and southwestern states. If you are curious about whether the rattlesnake vaccine is available in your area, check with your local veterinarian.
How Does the Rattlesnake Vaccine Work?

According to the manufacturer, the vaccine works by creating antibodies that protect against rattlesnake venom, thereby neutralizing the venom if a dog ever does suffer a bite. The rattlesnake vaccine is only meant to protect against venom from the Western Diamondback Rattlesnake. It provides no protection against bites from coral snakes, water moccasins, or the Mojave Rattlesnake.
The vaccine manufacturers claim that dogs that have been properly inoculated with a rattlesnake vaccine suffer less pain and have a lower risk of permanent damage from bites. The important takeaway from this is that even if a dog has been vaccinated, the manufacturer states that it is still imperative to seek emergency veterinary care if your dog has been bitten.
It is important to note that there are no peer-reviewed studies that prove that this vaccine actually works, and a peer-reviewed study published in 2014 found that this vaccine did not provide any protection to dogs that had been bitten and required treatment with antivenom. In addition, a 2018 study suggests vaccination has been linked to anaphylaxis and lack of clinical protection in dogs who have been subsequently bitten by a rattlesnake.
Rattlesnake Vaccination Schedule for Dogs

Your veterinarian will be your best resource to answer questions that you have about the rattlesnake vaccine schedule and if this vaccine is recommended for your dog.
Manufacturer guidelines for the rattlesnake vaccine indicate that a dog should receive an initial vaccination and then a booster one month later, followed by annual vaccine boosters preferably in the spring before rattlesnake season peaks.
Manufacturer guidelines state that the vaccine should be given at least 30 days before any potential exposure to rattlesnakes, and if your dog is exposed to rattlesnakes for longer than 6 months, twice yearly boosters are recommended because the antibodies decline over time and the dog loses protection.
Precautions When Considering This Vaccine
You may have noticed there is some controversy surrounding this vaccine in the veterinary community, or you may have been told by your veterinarian that she doesn’t recommend the vaccine because there are no controlled studies proving its efficacy.
There are anecdotal reports of dogs reacting less to snake bites with this vaccine, and there are reports that the vaccine made no difference, which can be confusing and subjective. In addition, there are no studies that prove that the dogs that reacted less to snakebites after vaccination were actually injected with venom from the bite. In fact, up to 30 percent of all snake bites can be dry bites, meaning that the snake did not inject any venom during the bite.
Furthermore, a pet parent may develop a false sense of security after having their dog vaccinated with a rattlesnake vaccine and decide not to seek immediate veterinary care if their dog is bitten, resulting in suffering and possible death. This vaccine should never be considered the sole means of protection against rattlesnake bites.
Dogs that have a history of vaccine reactions or dogs that are sick or have a condition that suppresses their immune system are not good candidates for the rattlesnake vaccine.
Manufacturers of the Rattlesnake Vaccine for Dogs
Rattlesnake vaccine is manufactured by one company, Red Rocks Biologics, based in Sacramento, California.
Cost of the Rattlesnake Vaccine for Dogs
The cost of a rattlesnake vaccine for dogs varies, and the price is set by your veterinary clinic. Prices can run anywhere from $30-$50 per booster, and may also require the cost of an examination as well ($40-$75).
Does Your Dog Need the Rattlesnake Vaccine?

Having your dog vaccinated with a rattlesnake vaccine is a very personal decision that can only be made by you, the pet parent, and must be based on your veterinarian’s recommendations.
It is critical to realize that even if your dog receives this vaccine, if your dog is bitten, the vaccine will not make your dog immune to the snake venom. At most, it may buy you some time so you can transport your dog to the veterinary hospital, and it may lessen some symptoms. Anytime a dog is bitten, you must seek immediate emergency veterinary care.
If your dog is routinely exposed to places where rattlesnakes live, then the vaccine may be helpful for your dog, however, that is a decision that you must make under the guidance of and in partnership with your local veterinarian. Together, you make up your dog’s health care team, and your veterinarian can help you make informed decisions about the health and wellness of your dog.
Bordetella Vaccine for Dogs
- 2020-05-29T15:43:20
- Natalie Marks, DVM
A large part of a veterinarian’s role is keeping our canine patients healthy and protecting them from disease that can transmit to humans in the household. Veterinarians also evaluate environmental risks and recommend individual vaccination strategies to protect our pets when they are out in the community.
We want to know what exposure your pet has on a daily basis. Does your dog go to communal dog spaces? Does he socialize in dog runs or public parks? Does your dog have regular grooming appointments? Does he go to training classes or boarding facilities?
If you’ve answered yes to any or all of these questions, your dog is at risk of contagious respiratory diseases caused by the Bordetella bacteria—the most common being kennel cough.
This disease can cause a lingering cough and decrease in appetite in adult dogs and serious disease like pneumonia in puppies and dogs with compromised immune systems. But the Bordetella vaccine for dogs can help protect your pup from kennel cough and other respiratory diseases.
What is the Bordetella Vaccine?
The canine Bordetella vaccine helps to protect against infection from a bacterium called Bordetella bronchiseptica. This vaccine was created to be given to dogs that are considered socially active. This includes dogs that go to groomers, boarding facilities, dog parks, daycares, training classes, live in large apartment communities, and those that participate in pet therapy.
The Bordetella vaccine protects dogs against kennel cough. This leads to some confusion around the naming of the vaccine. But the kennel-cough nickname originated because many of the cases of this disease were dogs that were frequently boarded. However, this disease can impact any socially active dog, not just those in boarding facilities.
This vaccine can be given orally, intranasally (through the nose), or with an injection. It is administered in all small animal clinics, but also routinely given at shelters, humane societies, rescues, government-run animal groups, and even by some breeders.
How Does it Work?
As veterinarians learned more about this bacterium, we found that Bordetella alone does not create the kennel cough disease. In fact, experts learned that affected dogs first had to become infected with a virus called parainfluenza.
This is NOT to be confused with canine influenza, or the dog “flu.” Parainfluenza virus causes the little hairs (or cilia) inside a dog’s trachea (or windpipe) to become paralyzed. Why is this so important? Well, these hairs are responsible for flicking bacteria upward and outward away from the lungs to help prevent respiratory disease. But, when those hairs can’t work temporarily, Bordetella bacteria has an unobstructed path into the respiratory system of the dog, causing cough and other signs.
Because of this knowledge, most effective Bordetella vaccines also have coverage against the parainfluenza virus too. So, this vaccine actually has dual protection!
Bordetella Vaccination Schedule for Dogs
With any vaccination, it’s always very important to talk to your veterinarian about your dog’s individual and environmental risk factors. That being said, according to the American Animal Hospital Association, the leading voice on vaccine protocols for small animal veterinarians in the United States, the recommended Bordetella vaccine schedule for puppies and dogs is as follows:
Puppies can be vaccinated with the intranasal (administered through the nose) vaccine as early as 3 weeks of age (depending on the product label). A second dose should be given two to four weeks later.
Alternatively, puppies can receive the injectable Bordetella vaccine starting at 6 to 8 weeks of age, followed by a booster between 10 and 12 weeks of age.
There is also an intraoral (administered into the cheek pouch) vaccine option for dogs 7 weeks of age or older.
For adult dogs or puppies older than 16 weeks, the intranasal vaccine can be given once, and the injectable vaccine should be given twice—2 to 4 weeks apart.
Adult dogs should then receive a booster every 6 to 12 months, depending on exposure risk.
Side Effects of the Bordetella Vaccine

Bordetella is considered a very safe vaccine for dogs in general, but just like with any vaccination given to any species, there are some general categories of side effects after vaccination.
Some of these side effects include:
Pain at the injection site. If the vaccine is given under the skin (subcutaneous), your dog may experience some pain at the site of the injection. This is usually temporary and goes away on its own without any intervention.
Sneezing or reverse sneezing. The Bordetella vaccine can be administered in the nostrils and some dogs may experience sneezing or reverse sneezing (a loud, repetitive, throat-clearing noise) for a few minutes after the vaccination. While noticeable, this side effect usually resolves quickly.
Sluggishness and a slight appetite decrease. After any subcutaneous vaccination, some dogs may experience a small amount of sluggishness or inappetence for a short period of time. These signs should go away on their own. If they do not, contact your veterinarian.
In very rare instances, dogs—just like people—can have anaphylactic reactions to vaccination, which is a life-threatening allergic reaction to the vaccine. If your dog starts to vomit, develops hives (red, raised itchy bumps on the body), develops swelling around the face and eyes, has difficulty breathing, or collapses, seek out veterinary care immediately. Signs of allergic reactions typically happen within 10-30 minutes of receiving the vaccine.
Manufacturers of the Bordetella Vaccine for Dogs
There are several manufacturers of Bordetella vaccines today. Some of these vaccines also protect against the canine parainfluenza virus and the canine adenovirus.
| Manufacturer | Product Name | Product Type | Protects Against |
| Boehringer Ingelheim | Recombitek | Oral | Bordetella bronchiseptica |
| Elanco | Bronchi-Shield Oral | Oral | Bordetella bronchiseptica |
| Elanco | Bronchi-Shield III | Intranasal | Bordetella bronchiseptica, Canine Parainfluenza Virus, Canine Adenovirus 2 |
| Merck Animal Health | Intra-Trac3 | Intranasal | Bordetella bronchiseptica, Canine Parainfluenza Virus, Canine Adenovirus 2 |
| Zoetis | Vanguard B Oral | Oral | Bordetella bronchiseptica |
| Zoetis | Vanguard B (IN) | Intranasal | Bordetella bronchiseptica |
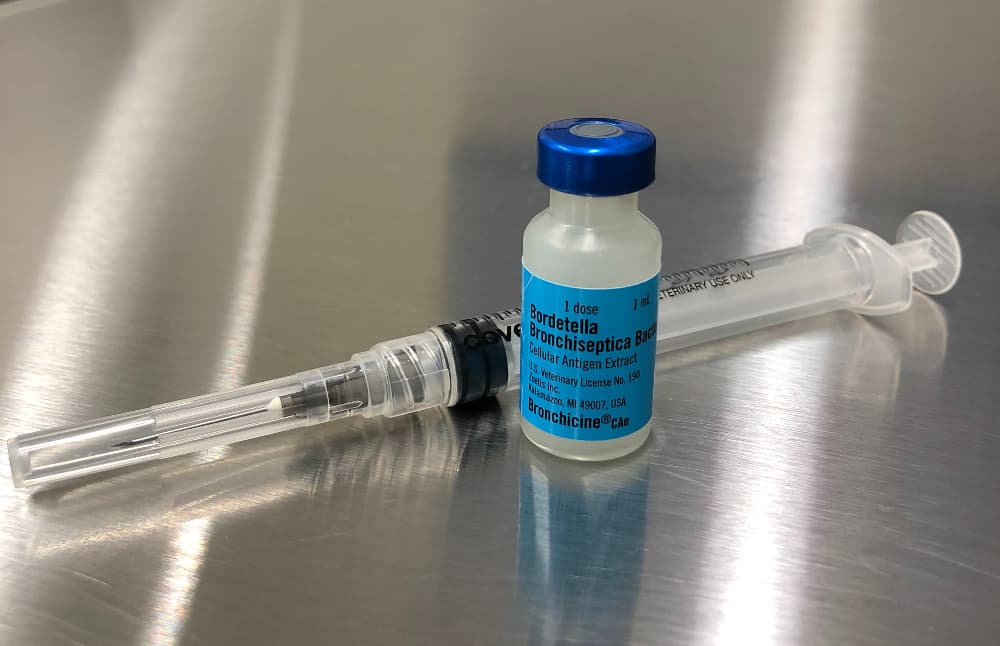
| Zoetis | Bronchicine CAe | Injectable | Bordetella bronchiseptica |
| Merck Animal Health | Nobivac Intra-Trac Oral Bb | Intraoral | Bordetella bronchiseptica |
What is the major difference between the oral, intranasal and injectable versions? All of these vaccine types work, but the selection process is also determined by how fast we need protection, the stress level of the dog for administration and the underlying health of the pet.
The intranasal and oral vaccines do work and protect faster, and they are a great choice if your dog needs to go to a boarding facility within a few days of vaccination. However, if you have more time and planning before a boarding event, the injectable vaccine is a good option and provides longer lasting immunity. And, as mentioned, some dogs are not comfortable with oral or intranasal administration of a vaccine, and that may make injectable versions more appropriate.
Cost of the Bordetella Vaccine for Dogs
In most locations around the country, this vaccine varies in cost from $20-$45 depending on the route of administration (injectable vs intranasal) and the average cost of veterinary care per region.
Does Your Dog Need This Vaccine?

Remember, the dogs most susceptible to kennel cough are the socially active dogs in the community and dogs that have a weaker immune system because of disease or current medications. If your dog frequently goes to a boarding facility, groomer, training classes, or does pet therapy, the recommendation is to have your veterinarian vaccinate your dog using the Bordetella vaccine.
As always, please talk to your veterinarian. He or she knows your dog and your lifestyle best and will help you make the most informed decision about the health of your best friend.
Leptospirosis Vaccine for Dogs: Everything You Need to Know
- 2020-05-26T18:57:54
- Liz McCalley, DVM, CCRT
Leptospirosis is a disease caused by the Leptospira genus of bacteria. This bacteria is present worldwide and is capable of infecting a range of mammals, including humans, dogs and, rarely, cats. The disease is zoonotic, meaning it can spread from infected animals to humans. Dogs typically become infected by coming into contact with water or soil contaminated with wildlife urine.
In recent years, cases of canine leptospirosis have been on the rise. The bacteria is more common in warmer and wetter climates. In the U.S., the Midwest, East, and Southwest are considered hotspots leptospirosis infections in dogs, but positive cases are reported nationwide.
USDA-approved leptospirosis vaccines are effective in the prevention of this disease in dogs.
What is the Leptospirosis Vaccine?
In the 1960s the first leptospirosis vaccines began to be administered to dogs in the United States and Europe. Since then, vaccination in dogs has become routine at many veterinary clinics across the U.S. However, not all clinics routinely perform or offer this vaccine. This is likely due to the vaccine’s non-core status as deemed by the World Small Animal Veterinary Association and the American Animal Hospital Association.
Given leptospirosis’ widespread prevalence and potential to cause death in dogs, many veterinarians disagree with the vaccine’s status as non-core. In fact, it may be considered a core vaccine depending on the area in which you live. For example, the UC Davis School of Veterinary Medicine’s hospital considers the lepto vaccine a core vaccine for dogs residing in the state of California.
The lepto vaccine is available from most general practice veterinary clinics throughout the United States. The law does not mandate vaccination anywhere in the U.S.
How Does the Lepto Vaccine for Dogs Work?

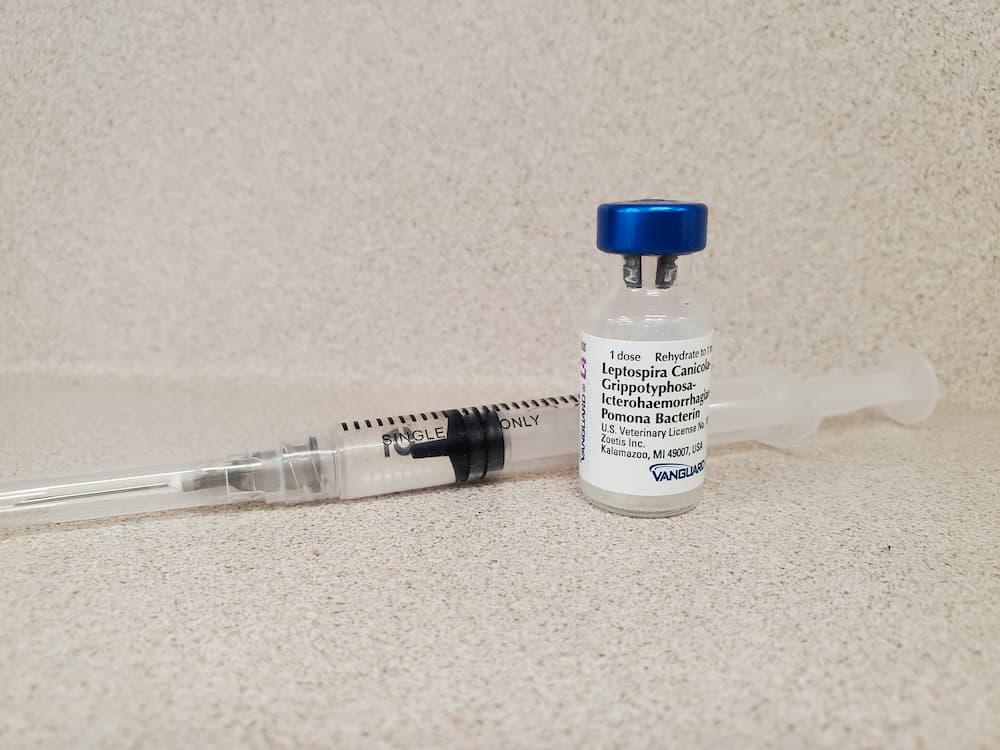
There are more than 250 strains of the leptospirosis-inducing bacteria. The bacteria are classified into different subspecies, called serovars, based on different proteins present on the surface of their cells. In the United States the bacteria from the four serovars—Cannicola, Icterohaemorrhagiae, Grippotyphosa, and Pomona—account for most, but not all, leptospirosis infections in dogs. For this reason, commercially available vaccines will not prevent against all possible causes of canine leptospirosis.
The first vaccines available only provided protection for two of the common serovars. The newer 4-way leptospirosis vaccines protect against infections from Leptospira bacteria in all four serovars. The veterinarian community now generally accepts that only the 4-way leptospirosis vaccine be given to dogs since it will provide the most protection against the disease.
The 4-way lepto vaccine contains inactivated pieces of the bacteria from the four different important serovars. Since the vaccine contains killed Leptospira bacteria, it will not cause leptospirosis in dogs who receive the vaccine. Once injected, the vaccine will prompt your dog’s immune system to produce antibodies which helps fight the Leptospira bacteria.
In order to produce a sufficient immune response, dogs must receive a booster vaccine 2 to 4 weeks following their first leptospirosis vaccine.
Leptospirosis Vaccine Schedule for Dogs

Puppies who are at risk of contracting leptospirosis can receive their first lepto shot as early as 8-9 weeks of age, but many experts recommend waiting until 12 weeks of age. Then, puppies should receive a booster vaccine 2 to 4 weeks later and then annually thereafter.
Adult dogs at risk of contracting leptospirosis should receive the vaccine annually. If an adult dog did not receive the shot as a puppy or she is significantly overdue for the vaccine, she will need a booster vaccine 2 to 4 weeks after the initial vaccine and then annually thereafter.
| First Lepto Shot | Second Lepto Shot | Third Lepto Shot | Additional Boosters |
| 9-12 weeks old | 11-16 weeks old | Approximately 1.5 years old | Once yearly |
Side Effects of the Leptospirosis Vaccine
Earlier versions of the leptospirosis vaccine reported higher risks for side effects than other common vaccines for dogs. However, newer production methods have significantly reduced the risk for adverse effects with two studies reporting between a 0.4 and 0.6 percent risk of reactions to the vaccine.
All injectable vaccines, including the lepto vaccine, will commonly produce mild side effects which typically resolve in one to two days. These include:
- Tiredness
- Soreness and mild swelling at the site of injection
If these symptoms persist beyond a few days or are causing your dog significant discomfort, you should contact your veterinarian.
Rarely, a leptospirosis vaccine may cause more serious side effects due to an allergic reaction, also known as a vaccine reaction. Symptoms of a leptospirosis vaccine reaction include:
- Vomiting
- Diarrhea
- Facial swelling
- Hives
- Difficulty breathing
- Collapse
- Injection site swelling
Most vaccine reactions in dogs will occur within a few hours of the vaccination. If your dog displays symptoms of a vaccine reaction, it is important to contact a veterinarian immediately. Most dogs experiencing a vaccine reaction will recover quickly with prompt veterinary care.
Prior to vaccinating your pet, it is important to notify your veterinarian if she has had a reaction to previous vaccines. For dogs with a history of mild vaccine reactions, a veterinarian may recommend administering medications prior to giving the lepto vaccine. For those with a history of serious reactions to prior vaccines, veterinarians generally do not recommend the leptospirosis vaccine.
According to the American Animal Hospital Association, separating the leptospirosis vaccine from the administration of other injectable vaccines, particularly in dogs weighing less than 22 lbs, may reduce the risk of an allergic reaction.
Manufacturers of the Lepto Vaccine for Dogs
The following leptospirosis vaccines are licensed for use in dogs in the United States:
| Manufacturer | Product Name |
| Zoetis | Vanguard L4 |
| Merck Animal Health | Nobivac Lepto4 |
| Elanco | Ultra Duramune 4L |
| Boehringer Ingelheim | 4Lepto |
Each of the above manufacturers also offers the lepto vaccine combined together with the DAPP core vaccine.
No one leptospirosis vaccine is currently regarded as safer or more effective than another.
All featured products were chosen at the discretion of the Great Pet Care editorial team and not directly recommended or endorsed by the author of this article. Great Pet Care may make a small affiliate commission if you click through and make a purchase.
Cost
The cost of a lepto vaccine for your dog can vary greatly depending on your location and whether you visit a low-cost vaccine clinic or a full service veterinary practice. The cost typically ranges from $15 to $35 for the lepto vaccine alone and may be up to $50-$60 for the combination DAPP with lepto vaccine.
If you have pet health insurance such as MetLife Pet Insurance, your plan may help cover some of the costs of vaccinations. Some plans offer preventative care or wellnes package add-ons that may cover expenses associated with keeping your pet healthy, such as certain vaccines, among many other healthcare perks.

- Get up to 90% of your bill reimbursed.
- No breed exclusions or upper age limits.
- Coverage for accidents start immediately.
Does Your Dog Need the Lepto Vaccine?
The question of whether or not to administer the leptospirosis vaccine routinely to all dogs is a hotly debated question amongst veterinarians. It is this author’s opinion that most dogs should receive this vaccine with very few exceptions, which include a history of previous allergic reactions to vaccines and indoor-only dogs.
Leptospirosis exists in rural, suburban, and urban settings across every state in the U.S. In urban environments, contact either directly or indirectly to rat or mice urine poses the biggest threat. In suburban environments, wildlife are a common source of infection. Finally, in rural areas, livestock and wildlife may transmit leptospirosis to dogs.
While hunting dogs, dogs that swim in lakes or ponds, and dogs living near farm animals are still thought to have a high risk of infection, a recent study found that dogs weighing less than 15 lbs had the highest likelihood of testing positive for lepto.
Here are some reasons to vaccinate your dog against leptospirosis:
- The disease can be severe and may result in death, especially if the disease is not rapidly diagnosed and treated.
- Leptospirosis is difficult to diagnose due to the wide ranges of symptoms, including asymptomatic carriers, and may go undetected. Because this disease can mimic many more common diseases, it is thought that leptospirosis often goes undiagnosed and the true rates of infections in dogs are likely much higher than reported rates.
- It is widespread throughout the U.S. and the rest of the world.
- Leptospirosis poses a risk to both your dog’s health and your health if your dog transmits the disease to you.
Lyme Vaccine for Dogs
- 2020-04-30T14:47:28
- Catherine Barnette, DVM
Lyme disease is a tick-borne infection, caused by the bacterium Borrelia burgdorferi. Lyme disease is found on multiple continents, including North America, Europe, and Asia. Within the U.S., Lyme disease was first observed in the Northeast and remains most common in that area; however, it is now found across much of the country.
Lyme disease is the most common tick-borne infection diagnosed in dogs in the United States. In 2022, 4 percent of canine blood samples sent to a reference laboratory for Lyme disease testing were positive for infection (1).
Clinical signs of Lyme disease vary significantly. In many dogs, Lyme disease is completely asymptomatic. These dogs show no signs of illness. Approximately 10 percent of infected dogs, however, develop clinical signs of Lyme disease several months after being bit by an infected tick (2). Common clinical signs of Lyme disease in dogs include fever, lethargy, and limping. Dogs with mild signs can typically be treated successfully with antibiotics. A small percentage of infected dogs go on to develop a serious kidney disease, known as Lyme nephritis, which can be fatal despite treatment.
What is the Lyme Disease Vaccine?
Although the syndrome now known as Lyme disease was first identified in human patients in 1975, Borrelia burgdorferi (the bacterium that causes the disease) was not identified until 1981. The first canine Lyme vaccine was introduced in 1992 (3).
The Lyme vaccine for dogs is available at most veterinary clinics, especially in areas where Lyme disease poses a significant threat. Even in low-risk areas, many veterinarians carry this vaccine in order to protect dogs traveling to Lyme-endemic areas. If your veterinarian does not carry this vaccine, they may be able to obtain it for you or direct you to another clinic where you can receive it.
This vaccine does not require a specialist visit and can often be administered with your dog’s other vaccinations at a routine wellness visit.
How Does the Lyme Vaccine for Dogs Work?

There are several different Lyme vaccines available, each made by different manufacturers. While these vaccines all differ slightly, each carries small amounts of the outer surface proteins found on Lyme bacteria. Some vaccines contain entire killed bacteria (including their outer surface proteins), while other vaccines contain only lab-created outer surface proteins. Regardless of the delivery format, it is these outer surface proteins that are primarily responsible for the body’s immune response.
When a dog receives a Lyme vaccine, the immune system develops antibodies against the outer surface proteins found in the vaccines. This primes the dog’s immune system to react to these proteins if they are encountered in the future. This reaction kills the bacteria, preventing infection.
One interesting characteristic of Lyme vaccines is that, in many cases, the vaccine acts within the tick instead of within the dog. Borrelia burgdorferi lives within the gut of an infected tick and is introduced to a dog via a tick bite. When a tick bites a dog, however, it also ingests the dog’s blood. This blood contains antibodies against B. burgdorferi, which immediately begin to attack the bacteria within the tick’s gut, instead of waiting for the bacteria to be introduced to the dog.
Lyme Vaccination Schedule for Dogs
An initial Lyme vaccine can be given as early as 8-9 weeks of age (depending on the manufacturer). After the initial vaccine, a booster vaccine must be given 3-4 weeks later. The dog is considered to be protected against Lyme disease four weeks after receiving the second Lyme vaccination.
For long-term protection, the Lyme vaccine must be repeated once annually for the remainder of your dog’s life. If your dog is significantly overdue for its annual booster, your veterinarian may recommend restarting the initial two-vaccine series.
| First Lyme Vaccine | First Booster Vaccine | Additional Boosters |
| 8-9 weeks old | 3-4 weeks later | Once annually thereafter |
Lyme Vaccine for Dogs: Side Effects

Vaccinations trigger a response from the immune system. Therefore, mild side effects are normal and expected. Expected effects may include a mild fever, lethargy, soreness at the site of the vaccine, and decreased appetite. Just like when you get a flu shot, your dog’s response to a vaccine may result in mild, short-lived signs of illness.
Occasionally, more serious reactions occur. Although severe vaccine reactions are rare, they require quick action. These reactions indicate an allergic reaction to a component of the vaccine.
Signs of an allergic reaction to Lyme vaccination include:
- Vomiting
- Diarrhea
- Hives
- Facial swelling
- Excessive itching (often of the face)
- Trouble breathing
- Extreme lethargy or weakness
- Collapse (due to anaphylactic shock)
If your dog experiences a vaccine reaction, contact your veterinarian immediately. Your veterinarian will help you determine whether your pet’s reaction can be managed at home or whether your dog needs emergency treatment. Once the immediate reaction has been addressed, your veterinarian will talk about future plans to decrease the likelihood of a similar reaction in the future.
Manufacturers of the Lyme Disease Vaccine for Dogs
There are five different Lyme vaccines licensed for use within the U.S.:
| Manufacturer | Product Name | Product Name |
| Zoetis | Vanguard® crLyme | LymeVax® |
| Merck | Nobivac® Lyme | |
| Elanco Animal Health | Duramune® Lyme | |
| Merial Animal Health | Recombitek® Lyme |
While there are slight differences in how these vaccines are produced and their mechanisms of action, all five are comparable in safety and efficacy.
Cost of the Lyme Disease Vaccine for Dogs
The Lyme vaccine typically costs $20-$40, depending on your location. Remember that your dog will need two vaccines the first year, then one vaccine yearly.
In order to administer the vaccine, your veterinarian will also likely need to perform a physical exam. Exam charges vary by geographic location, but typically range from $40-$80. In many cases, however, the Lyme vaccine is administered at a routine wellness visit, eliminating the need for a separate exam fee.
Does Your Dog Need the Lyme Vaccine?

The Lyme vaccine is a non-core vaccine. This means that it is not required for all dogs. Instead, the decision of whether to vaccinate a particular dog for Lyme disease is based on an individual risk assessment.
Dogs that are at higher risk of Lyme disease include:
- Dogs that live in high-risk areas (such as the northeastern U.S.)
- Dogs that travel to high-risk areas
- Dogs that are frequently exposed to ticks (through hiking, hunting, camping, etc.)
If your dog lives in or travels to the northeastern United States, your veterinarian is likely to highly recommend Lyme vaccination. If you live elsewhere in the country, your veterinarian’s recommendation will depend on your dog’s lifestyle. For example, a toy breed dog that eliminates on potty pads and never goes outdoors probably does not need a Lyme vaccine. A dog in a low-risk area that goes hiking regularly with its owner, however, may benefit from vaccination.
Lyme disease prevention in dogs requires more than just a vaccine, however. Like any other vaccine, Lyme vaccines are not 100 percent effective. In fact, tick control is shown to be more effective at preventing Lyme disease than vaccination alone (4). Therefore, any dog at risk of Lyme disease must be kept on an effective tick control, to help prevent not only Lyme disease but also other tick-borne diseases. In dogs at high risk of Lyme disease, however, vaccination provides an important backup layer of protection.